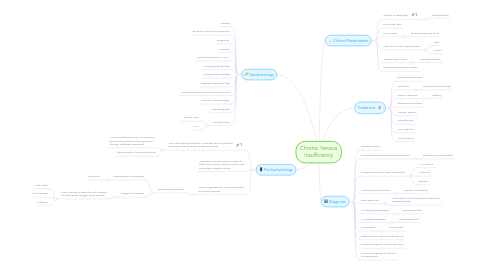
1. Epidemiology
1.1. Obesity
1.2. Excessive alcohol consumption
1.3. Pregnancy
1.4. Smoking
1.5. Previous leg trauma or DVT
1.6. Long periods standing
1.7. Long periods of sitting
1.8. Habitual crossing of legs
1.9. Constantly wearing constrictive garments
1.10. Previous Valve damage
1.11. Female gender
1.12. Family history
1.12.1. Varicose Veins
1.12.2. DVT
2. Pathophysiology
2.1. Vein valve damage leads to increased venous pressure of a large volume of blood against gravity
2.1.1. Venous swelling because of increased hydorstatic pressure pushing plasma through stretched vessel wall
2.1.2. Blood pools in lower extremities
2.2. Vessel wall remodeling secondary to altered connective tissue proteins and proteolytic enzyme activity
2.3. Venous hypertension, circulatory stasis, and tissue hypoxia
2.3.1. Inflammatory response
2.3.1.1. Fibrosclerotic remodeling
2.3.1.1.1. Ulceration
2.3.1.2. Sluggish Circulation
2.3.1.2.1. Poor clearing of waste by cells leading and decreased oxygen and nutrients
3. Clinical Presentation
3.1. Edema of lower legs
3.1.1. Pitting edema
3.2. Dry, rough skin
3.3. Pain in legs
3.3.1. Pt reports legs are tired
3.4. Alteration of skin pigmentation
3.4.1. Feet
3.4.2. Ankles
3.5. Venous stasis ulcers
3.5.1. Possible Infection
3.6. Decreased peripheral pulses
4. Treatment
4.1. Elevating extremities
4.2. TED hose
4.2.1. Compression Stockings
4.3. Physical exercise
4.3.1. Walking
4.4. Endovenous ablation
4.5. Surgical ligation
4.6. sclerotherapy
4.7. Vein resection
4.8. Vein stripping
5. Diagnosis
5.1. Detailed history
5.2. Comprehensive physical and assessment
5.2.1. Recollection of symptoms
5.3. Compare edema in lower extremities
5.3.1. 1-4+ edema
5.3.2. Unilateral
5.3.3. Bilateral
5.4. Assess peripheral pulses
5.4.1. Doppler if necessary
5.5. Tourniquet test
5.5.1. Noninvasive- test, Distinguish deep from superficial reflux
5.6. Photoplethysmography
5.6.1. Noninvasive test
5.7. Air plethysmography
5.7.1. Noninvasive test
5.8. Venography
5.8.1. Invasive test

