MYOCARDIAL INFARCTION
by Lina Hernandez
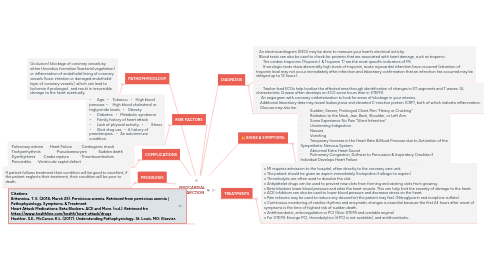
1. PATHOPHYSIOLOGY
1.1. Occlusion/ blockage of coronary vessels by either thrombus formation (bacterial vegetation) or inflammation of endothelial lining of coronary vessels (toxic irritation or damaged endothelial layer of coronary vessels), which can lead to Ischemia if prolonged , and result in irreversible damage to the heart eventually.
2. COMPLICATIONS
2.1. ·Pulmonary edema ·Heart Failure ·Cardiogenic shock ·Tachyarrhythmia ·Pseudoaneurysm ·Sudden death ·Dysrthythmia ·Cardia rapture ·Thromboembolism ·Pericarditis ·Ventricular septal defect
3. PROGNOSIS
3.1. If patient follows treatment their condition will be good to excellent, if the patient neglects their treatment, their condition will be poor to death.
4. Citations Britannica, T. E. (2018, March 29). Pernicious anemia. Retrieved from pernicious anemia | Pathophysiology, Symptoms, & Treatment Heart Attack Medications: Beta Blockers, ACE and More. (n.d.). Retrieved fro https://www.healthline.com/health/heart-attack/drugs Huether, S.E., McCance, K.L. (2017). Understanding Pathophysiology. St. Louis, MO: Elsevier.
5. RISK FACTORS
5.1. • Age. • Tobacco. • High blood pressure. • High blood cholesterol or triglyceride levels. • Obesity. • Diabetes. • Metabolic syndrome. • Family history of heart attack • Lack of physical activity. • Stress • Illicit drug use. • A history of preeclampsia. . • An autoimmune condition.
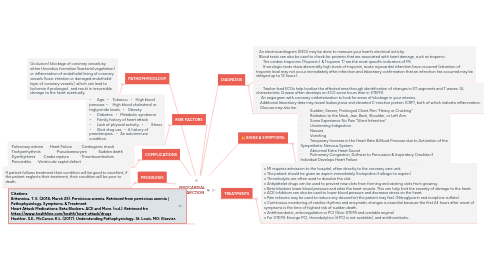
6. DIAGNOSIS
6.1. · An electrocardiogram (EKG) may be done to measure your heart’s electrical activity. · Blood tests can also be used to check for proteins that are associated with heart damage, such as troponin. · The cardiac troponins (Troponin I & Troponin T) are the most specific indicators of MI. · If serologic tests show abnormally high levels of troponin, acute myocardial infarction have occurred (elevation of troponin level may not occur immediately after infarction and laboratory confirmation that an infarction has occurred may be delayed up to 12 hours).
6.2. · Twelve-lead ECGs help localize the affected area through identification of changes in ST segments and T waves. (A characteristic Q wave often develops on ECG some hours later in STEMI). · An angiogram with coronary catheterization to look for areas of blockage in your arteries. · Additional laboratory data may reveal leukocytosis and elevated C-reactive protein (CRP), both of which indicate inflammation. · Glucose may also be elevated and the patient’s glucose tolerance may remain abnormal for several weeks.
7. SIGNS & SYMPTOMS:
7.1. · Sudden, Severe, Prolonged Chest Pain “Heavy or Crushing” · Radiation to the Neck, Jaw, Back, Shoulder, or Left Arm · Some Experience No Pain “Silent Infarction” · Unrelenting Indigestion · Nausea · Vomiting · Temporary Increase in the Heart Rate & Blood Pressure due to Activation of the Sympathetic Nervous System · Abnormal Extra Heart Sound · Pulmonary Congestion, Dullness to Percussion & Inspiratory Crackles if Individual Develops Heart Failure · Peripheral Vasoconstriction Causing Skin to become Cool & Clammy
8. TREATMENTS
8.1. v MI requires admission to the hospital, often directly to the coronary care unit. v The patient should be given an aspirin immediately (ticlopidine if allergic to aspirin) v Thrombolytic are often used to dissolve the clot. v Antiplatelet drugs can be used to prevent new clots from forming and existing clots from growing. v Beta-blockers lower blood pressure and relax the heart muscle. This can help limit the severity of damage to the heart. v ACE inhibitors can also be used to lower blood pressure and decrease stress on the heart. v Pain relievers may be used to reduce any discomfort the patient may feel. (Nitroglycerin and morphine sulfate). v Continuous monitoring of cardiac rhythms and enzymatic changes is essential because the first 24 hours after onset of symptoms is the time of highest risk of sudden death. v Antithrombotic, anticoagulation or PCI (Non-STEMI and unstable angina) v For STEMI: Emerge PCI, thrombolytics (if PCI is not available), and antithrombotic.