1. Data security, cybersecurity & access
1.1. Wearable devices, later adoption to allow maturity of technology and identification of security challenges
1.1.1. Serious consequences if devices are compromised (stealing data, changing records, changing settings, drug doses)
1.2. Removing identifiers doesn't mean that patient data remains anonymous (can combine data sets or records and identify people)
1.3. Where data is housed is how it is regulated. Data not stored in Canada means it isn't covered by Canadian privacy and data storage legislation
1.4. CIA acronym when it comes to cybersecurity
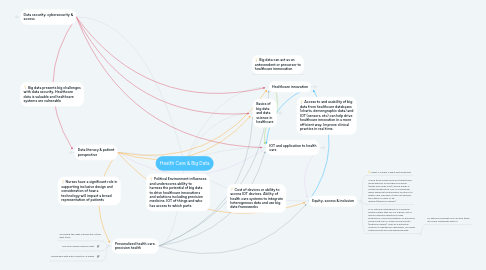
1.5. "94% of healthcare organizations have experienced at least one type of cyberattack" (Bhuyan, S., et al. 2020, p. 91)
1.5.1. data fraud mostly comes from insiders
1.5.1.1. Health data is high valuable and more prone to attack
1.5.2. Proactive approach, with focus on security processes and not specific technological fixes (Bhuyan, S., et al. 2020, p. 5)
1.6. Use of AI and machine learning to identify anomolies that could signal a cyber attack vs a reactive approach that identifies malware. Malware executables doubled between 2010-2012, making it challenging to be proactive
1.6.1. Security Risks:
1.6.1.1. threats
1.6.1.1.1. vulnerabilities
1.6.1.2. "A security incident is an act that threatens the confidentiality, integrity, or availability of information assets and systems" (Sarker, et al. 2020, p. 5)
1.6.2. Defense strategies
1.6.2.1. antivirus, firewalls, user authentication, access control, data encryption
1.6.2.1.1. anomaly based intrusion detection
2. Data literacy & patient perspective
2.1. Risling, T., & Low, C. (2019) Advocating for Safe, Quality and Just Care: what Nursing leaders need to know about artificial intelligence in healthcare delivery. Nursing Leadership. 31 (2), 31-43.
2.1.1. Nurses have essential knowledge and perspective to inform the development and integration of AI solutions in health care.
2.1.1.1. Nursing perspective is largely absent from AI design, development and implementation.
2.1.1.1.1. Integration of Nursing Informatics into curriculum is essential to ensure the expertise and knowledge of nursing is not discounted in AI design and application decisions
2.2. Risling.T., & Risling, D. (2020). Advancing nursing participation in user-centred design. 25 (3), 226-238.
2.2.1. Provides a framework for nursing expertise to be incorporated into user-centered design
2.2.1.1. Highlights the need for interdisciplinary collaboration and nurses to evolve their knowledge and understanding of user-centered design "the digitial health solution and design is driven by an understanding that the product is most likely to fulfill user needs when its development process is based on iterative cycles in which potential users are consulted early and often" (Risling & Risling, 2020, p. 228)
2.2.1.1.1. Nursing has opportunity to make design more diverse and more inclusive. Considering social determinants of health and how this impacts usability of a technology
2.3. Risling,T., M.J., et al. (2017). Evaluating patient empowerment in association with ehealth technology: scoping review. Journal of Medical Internet Research. 19 (9). 1-17.
2.3.1. Supporting patients to be e-health literate and consideration of in-equites in ability to develop e-health competencies and access.
2.3.1.1. Connect care will have an online patient portal. What about patients who do not have the IT infrastructure to access these platforms and personal health information? How will nursing support these patients? What is our role in design and implementation and ensure a broad representation of perspectives
2.3.1.1.1. How will nursing support health literacy as well as e-health literacy for patients, considering the influence of social determinants of health?
2.3.1.1.2. "Portals have been associated with small changes in patient empowerment and activation" (Risling, et al 2017, p. 8)
2.4. Patients are more and more becoming consumers and e-health literate. Expectations around informational continuity and reduction in fragmentation of care
3. Personalized health care, precision health
3.1. "providing the right intervention at the right time"
3.2. Precision health requires data
3.3. Challenges with data collection & usage
4. Political Environment influences and underscores ability to harness the potential of big data to drive healthcare innovations and solutions including precision medicine, IOT of things and who has access to which parts
5. Nurses have a significant role in supporting inclusive design and consideration of how a technology will impact a broad representation of patients
6. Big data presents big challenges with data security. Healthcare data is valuable and healthcare systems are vulnerable
7. Healthcare innovation
7.1. What is innovation?
7.1.1. "Something new, or perceived new by the population experiencing the innovation, that has the potential to drive change and redefine healthcare's economic and/or social potential" (Weberg, D. 2009. Innovation in Health Care, A concept Analysisi. Nurs Admin Q. 33 (3), 227-237.
7.2. Innovation is not the same as invention
8. IOT and application to health care
8.1. "network of physical devices and other items, embedded with electronics, software, sensors, and network connectivity which enables these objects to connect and exchange data" (Dimitrov, 2016, p. 156).
8.2. Challenges with IOT
8.2.1. Data security: how is data stored and how is it being accessed and by whom
8.2.1.1. Interoperability (ability of devices to communicate with each other, may not speak the same "language"
8.2.1.1.1. Fragmentation of health care data (exists in many formats) and is not collected in uniform ways
8.3. Opportunities
8.3.1. Assist in collection of dat from real world experience
8.3.1.1. aggregate data in an integrated database can inform real time care decisions
8.3.1.1.1. Engagement of patients in their care, with personal data at their fingertips. May promote more autonomy and adherence to treatment plans with real time feedback
9. Equity, access & inclusion
9.1. What is valued is what get measured
9.2. AI and technology fields are traditionally dominated by a homogenous group (white and Asian men), which brings a limited perspective. This is a challenge when applying technological solutions to health care, because it may not address the needs of users or be relevant(Kathrina Ingram)
9.3. AI or artificial intelligence is a machine based system that can for a given set of human-defined objectives make predictions, recommendations or decisions influencing real or virtual environments (Kathrina Ingram) seen as a potential solution to healthcare challenges, including cybersecurity and managing big data.
9.3.1. As Kathrina brought up in lecture there are some challenges with AI
10. Basics of big data and data science in healthcare
10.1. Characteristics of big data Volume (vast amounts of data), Velocity (speed at which data can be accessed and analyzed), Variability (various sources of data)
10.1.1. Big data can be messy, coming from multiple sources and are not linked. "with its diversity in format, type and context, it is difficult to merge big healthcare data into conventional database, making it enormously challenging to process"
10.2. Five data rights (Remus, S. & Donelle, L. (2019). Big Data: Why Should Canadian Nurse Leaders Care? Nursing Leadership. 32 (2), 19-30.
10.2.1. The right data
10.2.1.1. in the right amount
10.2.1.1.1. to the right person
10.2.2. Significant lags in knowledge translation, with 7-17 years between research being integrated into practice, meaning it's already outdated and limits ability to provide evidence informed practice effectively
