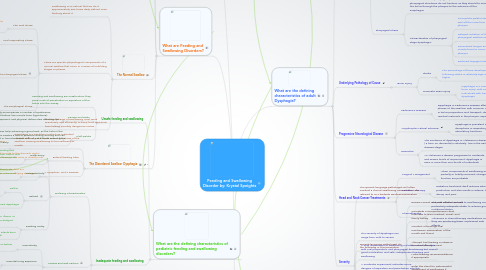
1. Introduction
1.1. Dysphagia
1.1.1. The impairment in the ability to swallow
1.1.2. Individuals with disruption in their swallowing ability may eating to be a burden
1.1.3. Dysphagia is a type of feeding disorder because the individual with dysphagia can no longer eat safely
1.1.4. Dysphagia occurs during the age spectrum for a variety of reasons due to development, neurological, or structural problems that alter the normal swallowing process
1.2. Oral-Motor System
1.2.1. Oral-Motor Functions
1.2.1.1. The strength and coordination of the articulators
1.2.2. Oral-Motor Muscular Tone
1.2.2.1. The tension and posture of the articulators
1.2.3. Oral-Motor Sensation
1.2.3.1. The sensitivity to taste, movement, and textures
2. What are Feeding and Swallowing Disorders?
2.1. Pediatric Feeding Disorders
2.1.1. The definition of a child with a feeding disorder is a persistent failure to eat adequately for a period of at least 1 month
2.1.2. Traits of a child with a feeding order:
2.1.2.1. Unsafe or inefficient swallowing patterns
2.1.2.2. Growth delay affecting height and/or weight
2.1.2.3. Lack of tolerance of food textures and tastes
2.1.2.4. Poor appetite regulation
2.1.3. Mild and transient feeding problems are common in young children; 25 to 35% of parents report that their young children have feeding issues
2.1.3.1. From the very start of their lives, many of these children exhibit significant impairments of feeding and require the earliest of interventions while in the Neonatal intensive care unit
2.2. Dysphagia
2.2.1. Deglutition
2.2.1.1. The complex neuromuscular act of moving substances from the oral cavity to the esophagus
2.2.2. Unsafe swallowing can be a life-or-death matter, as poor management and coordination of swallowing increases a child's or adult's risk of penetration and aspiration of food or liquid into the laryngeal area, which serves as the gateway to and the protector of the lungs
2.2.2.1. Penetration
2.2.2.1.1. Food or liquid enters the larynx, which can cause choking and respiratory distress
2.2.2.2. Aspiration
2.2.2.2.1. The food or liquid passes through the larynx and into the lungs, which can interfere with the exchange of air in the lungs and cause asphyxiation or a pulmonary infection
2.3. The Normal Swallow
2.3.1. Swallowing is so natural that we do it approximately 580 times daily without even thinking about it
2.3.2. There are specific physiological components of a normal swallow that occur in a series of unfolding stages or phases
2.3.2.1. The Oral Phase
2.3.2.1.1. The role of the oral phase is to move the bolus to the rear of the oral cavity and prepare it for propulsion down the throat
2.3.2.2. Oral Preparatory Phase
2.3.2.2.1. The role of the oral preparatory phase is to prepare the substance to be swallowed for swallowing
2.3.2.3. The Pharyngeal Phase
2.3.2.3.1. pharyngeal swallow reflex
2.3.2.3.2. Reflexive cough
2.3.2.3.3. Apneic moment
2.3.2.4. The Esophageal Phase
2.3.2.4.1. The esophageal phase moves the bolus through the esophagus into the stomach
2.3.3. The four phases of swallowing must work seamlessly and efficiently to keep food and drink from talking possibly dangerous routes
2.4. The Disordered Swallow: Dysphagia
2.4.1. Dysphagia is a condition is which an individual exhibits difficulty in at least one of the phase of the swallow, causing swallowing to be inefficient or unsafe
2.4.1.1. When swallowing, is unsafe, individuals are are risk of penetration or aspiration because of poor coordination or management of the bolus as it moves through the swallowing phases
2.4.1.1.1. Individuals with dysphagia may be unable to intake certain food consistencies safely and must have their diets changed or need to be fed through an alternative means
2.4.2. Enteral feeding tube
2.4.2.1. Directs a liquid formula to the stomach and is typically placed through the nose or directly into the stomach
2.4.3. A symptom, Not a Disease
2.4.3.1. Dysphagia is not a disease but rather is a symptom that results from an underlying etiology, or cause
3. What are the defining characteristics of pediatric feeding and swallowing disorders?
3.1. Unsafe feeding and swallowing
3.1.1. Feeding and swallowing are unsafe when they pose a risk of penetration or aspiration of the bolus into the airway
3.1.2. Causes and Risks
3.1.2.1. : Dysphagia frequently accompanies a number of syndromes, particularly those that feature low muscle tone (hypotonia), delayed motor development, and physical deformities affecting the oral-motor areas
3.1.3. Cleft palate
3.1.3.1. requires help achieving a good seal, as the hole in the palate creates a loss of pressure during sucking and can result in formula, breast milk, or solid foods entering the nasal cavity
3.2. Inadequate feeding and swallowing
3.2.1. Defining Characteristics
3.2.1.1. Inefficiency
3.2.1.1.1. Children who are inefficient at feeding and swallowing are unable to meet their caloric and nutritional needs, because the process is not productive
3.2.1.2. Overselectivity
3.2.1.2.1. Children with overselective eating patterns are restrictive in the taste, type, texture, or volume of food they will eat
3.2.1.3. Refusal
3.2.1.3.1. Reflux
3.2.1.3.2. Conditioned dysphagia
3.2.1.4. Feeding Delay
3.2.1.4.1. Because of developmental delays, illness, or trauma, some children experience delayed development of feeding skills
3.2.1.4.2. Low birth weight: infants born exceptionally small
3.2.2. Causes and Risk Factors
3.2.2.1. Prematurity
3.2.2.1.1. When a child is born at or before 37 weeks of gestation
3.2.2.2. Prenatal Drug Exposure
3.2.2.2.1. Prenatal exposure to alcohol, tobacco, cocaine, heroin, and other toxic substances has been linked to prematurity and low birth weight, as well as to longer-term growth failure and depressed neurological functioning, any one of which can impede a young child's feeding development and swallowing skills
3.2.2.3. Diet Restrictions
3.2.2.3.1. Some children are placed on strict or modified diets in response to diabetes, phenylketonuria (PKU), and other metabolic disorders
3.2.3. Inappropriate feeding and swallowing
3.2.3.1. Defining Characteristics
3.2.3.1.1. Children who exhibit inappropriate feeding behaviors demonstrate undesirable and disruptive behaviors during mealtimes
3.2.3.1.2. Inappropriate feeding behaviors include screaming, spitting, throwing, hitting, and other similar actions
3.2.3.2. Cause and Risk Factors
3.2.3.2.1. About one-third of feeding disorders in young children result from nonorganic causes
3.2.3.2.2. Many parents behaviors can undermine or impair the feeding relationships:
4. How are Pediatric feeding and swallowing disorders identified and treated?
4.1. Early Identification and Referral
4.1.1. The timely identification of pediatric feeding and swallowing disorders is critical so that immediate intervention can sustain the child's health and nutrition
4.1.1.1. Feeding problems emerge much earlier than referral typically occurs
4.1.1.2. When feeding problems persist, problematic secondary behaviors can emerge
4.2. Comprehensive Assessment
4.2.1. The speech-language pathologist will conduct a comprehensive assessment that includes a case history, a physical feeding/swallowing evaluation, and observation of mealtime interactions
4.2.1.1. Case History
4.2.1.1.1. The case history gathers information on the child's and family's eating and feeding experiences to explore possible manifestations of the disorder
4.2.1.2. Physical Feeding and Swallowing Evaluation
4.2.1.2.1. Following the case history, the specialist completes a careful evaluation of the structures and functions of the lips, tongue, jaw, teeth, and hard and soft palate
4.2.1.2.2. During the functional examination, the specialist ascertains both the safety and the efficiency of feeding and swallowing, as well as the quality of the intake
4.2.1.2.3. Modified barium swallow: video swallow study
4.3. Treatment Goals in Pediatric Feeding and Swallowing
4.3.1. The immediate and foremost goals of pediatric feeding and swallowing treatment are to ensure that nutritional needs are met for healthy growth and development and that feeding and swallowing do not endanger a child's life
4.3.2. Both physiological and psychological aspects of feeding and swallowing are targeted
4.3.2.1. Physiology of Feeding and Swallowing
4.3.2.1.1. Physiological targets emphasize the organic and neurodevelopment aspects if eating and drinking, such as muscle tone, articulatory movement and coordination, oral-motor sensitivity and body posture
4.3.2.1.2. Treatment focuses on improving the coordination of the swallow to achieve efficiency and safety
4.3.2.2. Psychology of Feeding and Swallowing
4.3.2.2.1. Psychological targets emphasize the behavioral aspects of eating and drinking such as accepting certain food types or textures, decreasing resistance and fussiness when eating, following a consistent meal schedule, and the like
4.3.2.2.2. Shaping is when the therapist moves a child incrementally toward a desired goal
4.3.2.2.3. Conditioning and reinforcement a child learns to associate a stimulus with a particular outcome, such as receiving a preferred food for eating a nonpreferred food
4.3.2.2.4. Systematic desensitization is when the therapist trains a child to accept an aversive sensory experience by breaking down into small steps and showing the child that each step is safe and possible
4.3.2.3. Alternative and Supplemental Feeding
4.3.2.3.1. Children who are candidates for supplement or alternative nutrition are those:
4.3.2.3.2. The most common solution is enteral, or tube, feeding, in which liquid nutrition is delivered through a tube
5. What are the defining characteristics of adult Dysphagia?
5.1. Phase Affected
5.1.1. Oral Preparatory Phase
5.1.1.1. Breakdowns in the oral oral preparatory phase occur when the structures and functions of the lips, tongue, cheeks, and mandible do not function as they should
5.1.1.2. Characteristics of oral preparatory phase dysphagia:
5.1.1.2.1. Decreased lip closure
5.1.1.2.2. Problems controlling the ingested materials
5.1.1.2.3. Difficulty biting or chewing
5.1.1.2.4. Inefficient oral preparation due to reduced range of motion of the tongue
5.1.1.2.5. Impaired sensitivity of the tongue, lips, and other oral structures
5.1.2. Oral Phase
5.1.2.1. The formed bolus moves posteriorly in the mouth toward the pharynx to trigger the swallow
5.1.2.2. Characteristics of oral phase dysphagia:
5.1.2.2.1. Difficulty moving the bolus to the pharynx
5.1.2.2.2. inability to adequately control the bolus flow
5.1.2.2.3. Delayed initiation of the bolus movement
5.1.3. Pharyngeal Phase
5.1.3.1. Breakdowns in the pharyngeal phase occur when the pharyngeal structures do not function as they should to move the bolus through the pharynx to the entrance of the esophagus
5.1.3.2. Characteristics of pharyngeal stage dysphagia:
5.1.3.2.1. Incomplete palatal elevation o seal off the nose from the pharynx
5.1.3.2.2. Delayed initiation of the pharyngeal swallow reflex
5.1.3.2.3. Diminished tongue and pharyngeal muscle force to move bolus through the pharynx
5.1.3.2.4. Reduced laryngeal elevation and closure
5.2. Underlying Pathology of Cause
5.2.1. Brain Injury
5.2.1.1. Stroke
5.2.1.1.1. The percentage of those developing dysphagia following stroke is relatively high 50% or even higher
5.2.1.2. Traumatic Brain Injury
5.2.1.2.1. Dysphagia is a common complication of traumatic brain injury, with one-fourth to three-fourth of individuals with traumatic brain injury exhibiting dysphagia
5.3. Progressive Neurological Disease
5.3.1. Parkinson's Disease
5.3.1.1. Dysphagia in Parkinson's Disease affects the oral, pharyngeal, and esophageal phases of the swallow, with common difficulties including drooling, abnormalities in bolus preparation and transport, delayed triggering of the swallow reflex, residual materials in the pharynx, aspiration, and diminished esophageal motility
5.3.2. Amyotrophic Lateral Sclerosis
5.3.2.1. Dysphagia is prevalent in ASL because of the disruptions in respiratory, phonatory, and articulatory functions
5.3.3. Dementia
5.3.3.1. The incidence of dysphagia in Alzheimer's disease ( a form on dementia) is relatively low in the early disease stages
5.3.3.2. As Alzheimer's disease progresses to moderate and severe levels of impairment, dysphagia is seen in more than one-fourth of individuals
5.4. Head and Neck Cancer Treatments
5.4.1. Surgical Management
5.4.1.1. When components of swallowing are either partially or totally removed, changes in swallowing function are probable
5.4.2. Radiation Therapy
5.4.2.1. Radiation treatment itself reduces saliva production and also results in edema, tooth decay, and pain
5.4.3. Chemotherapy
5.4.3.1. The side effects can lead to swallowing concerns, particularly adequate intake to achieve good nutritional status
5.4.3.2. Advances in chemotherapy medications mean they are producing fewer unpleasant side effects
5.5. Severity
5.5.1. The severity of dysphagia can range from mild to severe
5.5.2. A mild impairment of swallowing includes some difficulties with oral preparation and pharyngeal functioning but overall good mastication and safe, independent feeding and swallowing
5.5.3. A moderate impairment indicates some dangers of aspiration and penetration into the airway
5.5.4. A severe impairment indicates a serious risk of aspiration and penetration, and a profound impairment indicates that a person is unable to safely swallow
6. How is Adult Dysphagia identified and treated?
6.1. Clinical Swallowing Examination
6.1.1. The speech-language pathologist will often conduct a clinical swallowing examination, also referred to as a bedside swallow examination
6.1.2. Speech-language pathologist do the following in this procedure:
6.1.2.1. Review current and past medical records
6.1.2.2. Complete a comprehensive client interview to learn medical, social, and family history
6.1.2.3. Conduct a thorough oral mechanism examination of the mouth and throat
6.1.2.4. Attempt trial feeding or observe the client during a meal
6.1.2.5. Make feeding recommendations if appropriate
6.1.2.6. Refer the client for instrumental assessment of swallowing if indicated
6.1.2.7. Refer the client to to other professionals for any specialized testing that is needed
6.1.3. These five indicators suggest the need for instrumentation to quantify swallowing problems:
6.1.3.1. Clinical bedside findings are inconsistent with reported signs and symptoms of dysphagia
6.1.3.2. Instrumentation is needed to assist in determining the medical diagnosis
6.1.3.3. Dysphagia diagnosis or the safety and efficiency of the swallow require confirmation
6.1.3.4. Nutritional or pulmonary compromises are present
6.1.3.5. Specific swallowing information is required to design and implement a treatment plan
6.2. Instrumental Dysphagia Examination
6.2.1. Fiberoptic Endoscopic Examination
6.2.1.1. Provides direct visualization of the swallowing mechanism
6.2.1.2. A fiberoptic endoscope, a flexible tube containing a small camera, is passed through the nose and into the pharynx, yielding a real-time picture of swallowing, both before and after the swallow
6.2.2. Ultrasonography
6.2.2.1. The same technology long used to visualize a fetus in the mother's womb
6.2.2.2. In dysphagia evaluation, ultrasound uses high frequency sound waves to create a black-and-white picture of the structures targeted
6.2.3. Videofluoroscopy
6.2.3.1. The most commonly used instrumentation for swallowing evaluation and is the gold standard in most cases
6.2.3.2. Videofluoroscopy uses radiation, so client exposure must be considered and minimized
6.3. Treating Dysphagia
6.3.1. Compensatory Approaches
6.3.1.1. Compensatory approaches are strategies that compensate for a specific problem in order to make swallowing safe and efficient
6.3.1.2. Postural techniques are used quite commonly
6.3.1.3. Speech-language pathologist use diet modifications as a compensatory approach
6.3.2. Restorative Techniques
6.3.2.1. Are intended to improve or restore swallow function
6.3.2.2. The therapist might use thermal stimulation to improve the sensitivity of the oral area and the timeliness of the swallow reflex
6.4. Nutrition and Dietary Considerations
6.4.1. The importance of nutritional health to an individual with dysphagia cannot be overestimated
6.4.2. Some individuals are unable to meet their nutritional requirements orally so they need alternative nutritional means, such as a feeding tube
6.4.3. It is not unusual for dysphagia clients to receive both oral intake and tube feedings
