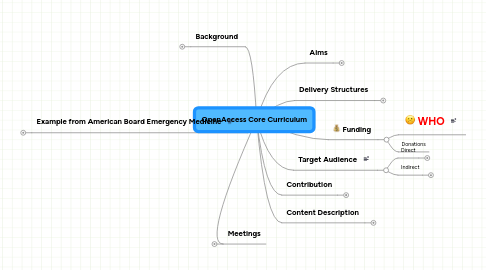
1. Background
1.1. Proposal for developing and disseminating a clinical toxicology curriculum
1.2. 400,000 deaths per year
1.3. Need
1.3.1. Universities
1.3.2. Hospitals
1.3.3. Regulatory
1.3.4. Geographic Variation
2. Meetings
2.1. Opportunistic
2.1.1. NACCT
2.1.2. EAPCCT
2.1.3. APAMT
2.2. Specific Meeting
2.2.1. Perhaps based on Contribution
2.3. Web Based
2.3.1. Wiki
2.3.2. Skype
2.3.3. Blog
3. Example from American Board Emergency Medicine
3.1. 1.0 Principles of Toxicology
3.1.1. 1.1 Pharmacology/Toxicology
3.1.1.1. 1.1.1 Pharmacokinetics/Toxicokinetics
3.1.1.2. 1.1.1.1 Bioavailability and Absorption
3.1.1.3. 1.1.1.2 Distribution
3.1.1.4. 1.1.1.3 Metabolism
3.1.1.5. 1.1.1.4 Elimination
3.1.1.6. 1.1.1.5 Clearance
3.1.1.7. 1.1.1.6 Models (eg, compartmental, physiologic)
3.1.1.8. 1.1.2 Pharmacodynamics/Toxicodynamics
3.1.1.9. 1.1.2.1 Dose/Concentration Relationship to Effect
3.1.1.10. 1.1.2.2 Structure-Activity Relationship
3.1.1.11. 1.1.2.3 Receptor Agonism/Antagonism
3.1.1.12. 1.1.2.4 Receptor Regulation
3.1.1.13. 1.1.3 Adverse Effects
3.1.1.14. 1.1.3.1 Mechanistic (predictable)
3.1.1.15. 1.1.3.2 Idiosyncratic
3.1.1.16. 1.1.4 Interactions
3.1.1.17. 1.1.4.1 Xenobiotic-Environment
3.1.1.18. 1.1.4.2 Xenobiotic-Food
3.1.1.19. 1.1.4.3 Xenobiotic-Xenobiotic (eg, drug-drug)
3.1.1.20. 1.1.5 Proteomics
3.1.1.21. 1.1.6 Tolerance and Withdrawal
3.1.1.22. 1.1.6.1 Behavioral Tolerance
3.1.1.23. 1.1.6.2 Biologic Tolerance
3.1.1.24. 1.1.7 Immunologic Response (eg, antibodies, cytokines)
3.1.1.25. 1.1.8 Pharmacogenomics/Toxicogenomics (eg, xenobiotic response, gene expression profiling)
3.1.2. 1.2 Molecular Components/Mechanisms
3.1.2.1. 1.2.1 Glycolysis and Oxidative Phosphorylation
3.1.2.2. 1.2.2 Other Metabolic Pathways (eg, amino acids and urea cycle)
3.1.2.3. 1.2.3 Membranes
3.1.2.4. 1.2.4 Enzymes and Transport Proteins (eg, methemoglobin, G6PD)
3.1.2.5. 1.2.5 Channels and Pumps
3.1.2.6. 1.2.6 Signal Transduction
3.1.2.7. 1.2.6.1 Receptor Isoforms and Subtypes
3.1.2.8. 1.2.6.2 Regulation and Messengers
3.1.2.9. 1.2.6.3 Neurotransmitters
3.1.3. 1.3 Cytotoxic Mechanisms (eg, apoptosis, microtubular dysfunction)
3.1.4. 1.4 Mutagenesis and Carcinogenesis
3.1.4.1. 1.4.1 Mutagenesis
3.1.4.1.1. 1.4.1.1 Chromosome Aberrations (structural, numeric)
3.1.4.1.2. 1.4.1.2 Gene Mutation (oncogenes, tumor suppressor genes)
3.1.4.2. 1.4.2 Development of Neoplasia
3.1.4.2.1. 1.4.2.1 Initiation (eg, genotoxic mechanisms)
3.1.4.2.2. 1.4.2.2 Procarcinogens and Conversion to Carcinogens (eg,
3.1.4.2.3. 1.4.2.3 Progression (eg, growth, invasiveness)
3.1.4.2.4. 1.4.2.4 Promotion (eg, nongenotoxic mechanisms biotransformation))
3.1.4.3. 1.4.3 Inhibition of Carcinogenesis-Modulating Factors
3.1.4.3.1. 1.4.3.1 Endogenous Factors (eg, age, sex, immune status, hormones)
3.1.4.3.2. 1.4.3.2 Exogenous Factors (eg, diet, radiation)
3.1.4.4. 1.4.4 Interactive Carcinogenesis
3.1.4.4.1. 1.4.4.1 Xenobiotic: Gene Interactions
3.1.4.4.2. 1.4.4.2 Xenobiotic: Physical Interactions
3.1.4.4.3. 1.4.4.3 Xenobiotic: Radiation Interactions
3.1.4.4.4. 1.4.4.4 Xenobiotic: Viral Interactions
3.1.5. 1.5 Adverse Reproductive and Developmental Outcomes
3.1.5.1. 1.5.1 Conception Impairment, Mutagenesis, and Teratogenesis
3.1.5.1.1. 1.5.1.1 Chromosomal and Gene Abnormalities
3.1.5.1.2. 1.5.1.2 Effects on Gametogenesis and Gametes
3.1.5.1.3. 1.5.1.3 Effects on Gonads
3.1.5.1.4. 1.5.1.4 Spontaneous Abortion and Perinatal Death
3.1.5.2. 1.5.2 Factors Determining Fetal or Infant Exposure to Agents
3.1.5.2.1. 1.5.2.1 Breast Milk Transfer
3.1.5.2.2. 1.5.2.2 Placental Transfer
3.1.5.2.3. 1.5.2.3 Xenobiotic Disposition (eg, maternal xenobiotic disposition, feta pharmacokinetics)l
3.1.5.3. 1.5.3 Offspring Effects
3.1.5.3.1. 1.5.3.1 Cancer
3.1.5.3.2. 1.5.3.2 Congenital Anomalies and Malformations
3.1.5.3.3. 1.5.3.3 Development of Infant/Child
3.1.5.3.4. 1.5.3.4 Genetic Mutations
3.2. 2.0 Toxins and Toxicants
3.2.1. 2.1 Drugs
3.2.1.1. 2.1.1 Analgesics, Anti-inflammatory Drugs
3.2.1.2. 2.1.1.1 Acetaminophen
3.2.1.3. 2.1.1.2 Nonsteroidal Anti-inflammatory Drugs
3.2.1.4. 2.1.1.3 Opioids
3.2.1.5. 2.1.1.4 Salicylates
3.2.1.6. 2.1.1.5 Others (eg, antigout drugs, gold)
3.2.1.7. 2.1.2 Antimicrobials
3.2.1.8. 2.1.2.1 Antibiotics
3.2.1.9. 2.1.2.2 Antifungals
3.2.1.10. 2.1.2.3 Antimycobacterials
3.2.1.11. 2.1.2.4 Antiparasitics
3.2.1.12. 2.1.2.5 Antiprotozoals
3.2.1.13. 2.1.2.6 Antiretrovirals
3.2.1.14. 2.1.2.7 Antiseptics
3.2.1.15. 2.1.2.8 Antivirals
3.2.1.16. 2.1.3 Chemotherapeutic Drugs
3.2.1.17. 2.1.3.1 Alkylators
3.2.1.18. 2.1.3.2 Antimetabolites
3.2.1.19. 2.1.3.3 Hormones
3.2.1.20. 2.1.3.4 Natural Drugs, (eg, vinca alkaloids, antibiotics)
3.2.1.21. 2.1.3.5 Miscellaneous (eg, platinum, hydroxyurea)
3.2.1.22. 2.1.4 Diagnostic Drugs (eg, radionuclides)
3.2.1.23. 2.1.5 Drugs That Affect Cholesterol and Lipids
3.2.1.24. 2.1.6 Drugs That Affect the Cardiovascular System
3.2.1.25. 2.1.6.1 Antidysrhythmics
3.2.1.26. 2.1.6.1.1 Calcium channel blockers
3.2.1.27. 2.1.6.1.2 Cardiac glycosides
3.2.1.28. 2.1.6.1.3 Potassium channel blockers
3.2.1.29. 2.1.6.1.4 Sodium channel blockers
3.2.1.30. 2.1.6.2 Antihypertensives
3.2.1.31. 2.1.6.2.1 Angiotensin system modulators
3.2.1.32. 2.1.6.2.2 -Adrenergic (and mixed , ) antagonists
3.2.1.33. 2.1.6.2.3 Centrally acting receptor agonists
3.2.1.34. 2.1.6.2.4 Diuretics
3.2.1.35. 2.1.6.2.5 Vasodilators (eg, nitrates, nitrites)
3.2.1.36. 2.1.6.3 Inotropes
3.2.1.37. 2.1.7 Drugs That Affect the Endocrine System
3.2.1.38. 2.1.7.1 Antidiabetic Drugs
3.2.1.39. 2.1.7.1.1 Insulin
3.2.1.40. 2.1.7.1.2 Oral hypoglycemics
3.2.1.41. 2.1.7.1.3 Others (eg, metformin, glitazones)
3.2.1.42. 2.1.7.2 Bone Active Drugs (eg, calcitonin, bisphosphonates)
3.2.1.43. 2.1.7.3 Electrolytes and Minerals
3.2.1.44. 2.1.7.4 Glucocorticoids
3.2.1.45. 2.1.7.5 Sex Hormones, Growth Hormones, and Anabolic Steroids
3.2.1.46. 2.1.7.6 Thyroid Drugs
3.2.1.47. 2.1.7.7 Vasopressin and Somatostatin Analogues
3.2.1.48. 2.1.8 Drugs That Affect the Gastrointestinal System
3.2.1.49. 2.1.8.1 Antidiarrheals
3.2.1.50. 2.1.8.2 Antiemetics
3.2.1.51. 2.1.8.3 Drugs Used for Biliary and Pancreatic Diseases (eg, bile salts,
3.2.1.52. pancreatic enzymes)
3.2.1.53. 2.1.8.4 Drugs Used for Inflammatory Bowel Disease
3.2.1.54. 2.1.8.5 Drugs Used to Treat Acid-Peptic Diseases
3.2.1.55. 2.1.8.6 Laxatives
3.2.1.56. 2.1.8.7 Promotilics
3.2.1.57. 2.1.9 Drugs That Affect the Hematologic System
3.2.1.58. 2.1.9.1 Anticoagulants
3.2.1.59. 2.1.9.2 Antifibrinolytics
3.2.1.60. 2.1.9.3 Antiplatelet Drugs
3.2.1.61. 2.1.9.4 Blood-Stimulating Drugs (eg, erythropoietin)
3.2.1.62. 2.1.9.5 Drugs Used to Treat Bleeding (eg, clotting factors, antiplasmin
3.2.1.63. drugs)
3.2.1.64. 2.1.9.6 Iron
3.2.1.65. 2.1.9.7 Thrombolytics
3.2.1.66. 2.1.10 Drugs That Affect the Immune System (eg, interferon, cyclophos-
3.2.1.67. phamide)
3.2.1.68. 2.1.10 Drugs That Affect the Immune System (eg, interferon, cyclophos-
3.2.1.69. phamide)
3.2.1.70. 2.1.11 Drugs That Affect the Nervous System
3.2.1.71. 2.1.11.1 Anesthetics
3.2.1.72. 2.1.11.1.1 Inhalational and sedative anesthetics (eg, nitrous oxide,
3.2.1.73. propofol)
3.2.1.74. 2.1.11.1.2 Local anesthetics
3.2.1.75. 2.1.11.2 Anticonvulsants
3.2.1.76. 2.1.11.3 Antiparkinsonism Drugs
3.2.1.77. 2.1.11.4 Drugs That Affect Autonomic Homeostasis
3.2.1.78. 2.1.11.4.1 Anticholinergics
3.2.1.79. 2.1.11.4.2 Antihistamines
3.2.1.80. 2.1.11.4.3 Antiserotonergics
3.2.1.81. 2.1.11.4.4 Cholinergics (eg, nicotine)
3.2.1.82. 2.1.11.4.5 Ergot and derivatives
3.2.1.83. 2.1.11.4.6 Methylxanthines
3.2.1.84. 2.1.11.4.7 Serotonin agonists and other proserotonergics (eg, dextro-
3.2.1.85. methorphan)
3.2.1.86. 2.1.11.4.8 Sympathomimetics (eg, amphetamines, cocaine)
3.2.1.87. 2.1.11.5 Ethanol
3.2.1.88. 2.1.11.6 Muscle Relaxants
3.2.1.89. 2.1.11.7 Neuromuscular Blockers
3.2.1.90. 2.1.11.8 Psychoactive Drugs and Hallucinogens (eg, marijuana, lysergic
3.2.1.91. acid diethylamide [LSD])
3.2.1.92. 2.1.11.9 Psychotropics
3.2.1.93. 2.1.11.9.1 Anxiolytics and sedative-hypnotics
3.2.1.94. 2.1.11.9.2 Antidepressants
3.2.1.95. 2.1.11.9.3 Antipsychotics
3.2.1.96. 2.1.11.9.4 Mood stabilizers
3.2.1.97. 2.1.12 Pharmaceutical Additives (eg, excipients)
3.2.1.98. 2.1.13 Veterinary Products
3.2.1.99. 2.1.14 Vitamins
3.2.2. 2.2 Industrial, Household, and Environmental Toxicants
3.2.2.1. 2.2.1 Airborne Solids
3.2.2.1.1. 2.2.1.1 Asbestos
3.2.2.1.2. 2.2.1.2 Coal Dust
3.2.2.1.3. 2.2.1.3 Organic Dust
3.2.2.1.4. 2.2.1.4 Silica
3.2.2.1.5. 2.2.1.5 Other Minerals (eg, man-made mineral fibers)
3.2.2.2. 2.2.2 Cleansers and Caustics
3.2.2.2.1. 2.2.2.1 Acids
3.2.2.2.2. 2.2.2.2 Alkali
3.2.2.2.3. 2.2.2.3 Bleach
3.2.2.2.4. 2.2.2.4 Detergents and Soaps
3.2.2.2.5. 2.2.2.5 Disinfectants and Topical Anti-infectives
3.2.2.2.6. 2.2.2.6 Swimming Pool Products
3.2.2.3. 2.2.3 Food Additives (eg, monosodium glutamate, sulfites)
3.2.2.4. 2.2.4 Household Products
3.2.2.4.1. 2.2.4.1 Aquarium Products
3.2.2.4.2. 2.2.4.2 Art Products
3.2.2.4.3. 2.2.4.3 Batteries
3.2.2.4.4. 2.2.4.4 Cosmetics
3.2.2.4.5. 2.2.4.5 Dental Products
3.2.2.4.6. 2.2.4.6 Hair Products
3.2.2.4.7. 2.2.4.7 Personal Hygiene Products
3.2.2.5. 2.2.5 Hydrocarbons/Solvents/Fuels
3.2.2.5.1. 2.2.5.1 Aldehydes
3.2.2.5.2. 2.2.5.2 Alcohols and Glycols
3.2.2.5.3. 2.2.5.3 Aliphatic Hydrocarbons
3.2.2.5.4. 2.2.5.4 Aromatic Hydrocarbons
3.2.2.5.5. 2.2.5.5 Halogenated Hydrocarbons
3.2.2.6. 2.2.6 Metals/Metalloids
3.2.2.6.1. 2.2.6.1 Arsenic (including arsine)
3.2.2.6.2. 2.2.6.2 Barium
3.2.2.6.3. 2.2.6.3 Beryllium
3.2.2.6.4. 2.2.6.4 Cadmium
3.2.2.6.5. 2.2.6.5 Chromium
3.2.2.6.6. 2.2.6.6 Cobalt
3.2.2.6.7. 2.2.6.7 Copper
3.2.2.6.8. 2.2.6.8 Lead
3.2.2.6.9. 2.2.6.9 Manganese
3.2.2.6.10. 2.2.6.10 Mercury
3.2.2.6.11. 2.2.6.11 Nickel
3.2.2.6.12. 2.2.6.12 Thallium
3.2.2.7. 2.2.7 Pesticides
3.2.2.7.1. 2.2.7.1 Fumigants and Sterilants
3.2.2.7.2. 2.2.7.2 Fungicides
3.2.2.7.3. 2.2.7.3 Herbicides
3.2.2.7.4. 2.2.7.4 Insecticides and Repellents
3.2.2.7.5. 2.2.7.4.1 Carbamates
3.2.2.7.6. 2.2.7.4.2 DEET
3.2.2.7.7. 2.2.7.4.3 Moth balls
3.2.2.7.8. 2.2.7.4.4 Organochlorines
3.2.2.7.9. 2.2.7.4.5 Organophosphates
3.2.2.7.10. 2.2.7.4.6 Pyrethrins and pyrethroids
3.2.2.7.11. 2.2.7.5 Rodenticides
3.2.2.7.12. 2.2.7.5.1 Anticoagulant
3.2.2.7.13. 2.2.7.5.2 Nonanticoagulant
3.2.2.7.14. 2.2.7.6 Other (eg, molluscides)
3.2.2.8. 2.2.8 Pollutants
3.2.2.8.1. 2.2.8.1 Air Pollutants (eg, respirable particulates)
3.2.2.8.2. 2.2.8.2 Persistent Organic Pollutants (eg, polychlorinated biphenyls, dibenzodioxins)
3.2.2.8.3. 2.2.8.3 Water Pollutants (eg, trihalomethanes)
3.2.2.9. 2.2.9 Toxic Gases
3.2.2.9.1. 2.2.9.1 Cellular Asphyxiant Gases
3.2.2.9.2. 2.2.9.2 Irritant Gases
3.2.2.9.3. 2.2.9.3 Radon
3.2.2.9.4. 2.2.9.4 Simple Asphyxiants (eg, methane, nitrogen)
3.2.2.9.5. 2.2.9.5 Smoke Inhalation
3.2.2.10. 2.2.10 Miscellaneous Toxicants
3.2.2.10.1. 2.2.10.1 Acrolein
3.2.2.10.2. 2.2.10.2 Acrylamides
3.2.2.10.3. 2.2.10.3 Acrylates
3.2.2.10.4. 2.2.10.4 Amines
3.2.2.10.5. 2.2.10.5 Aniline Compounds
3.2.2.10.6. 2.2.10.6 Azides
3.2.2.10.7. 2.2.10.7 Bromide Compounds
3.2.2.10.8. 2.2.10.8 Butadienes
3.2.2.10.9. 2.2.10.9 Carbon Disulfide
3.2.2.10.10. 2.2.10.10 Chlorates
3.2.2.10.11. 2.2.10.11 Coal Tar Products
3.2.2.10.12. 2.2.10.12 Diamines
3.2.2.10.13. 2.2.10.13 Dibromochloropropane (DBCP)
3.2.2.10.14. 2.2.10.14 Dimethylacetamide (DMAC)
3.2.2.10.15. 2.2.10.15 Dimethylformamide (DMF)
3.2.2.10.16. 2.2.10.16 Dinitrobenzene
3.2.2.10.17. 2.2.10.17 Dinitrotoluene (DNT)
3.2.2.10.18. 2.2.10.18 Epichlorohydrin
3.2.2.10.19. 2.2.10.19 Ethylene Dibromide (EDB)
3.2.2.10.20. 2.2.10.20 Ethylenediamine (EDA)
3.2.2.10.21. 2.2.10.21 Fluoride Compounds
3.2.2.10.22. 2.2.10.22 Fuels
3.2.2.10.23. 2.2.10.23 Hexachloro-1,3-Butadiene (HCBD)
3.2.2.10.24. 2.2.10.24 Isocyanates (eg, toluene diisocyante)
3.2.2.10.25. 2.2.10.25 Maleic Anhydride
3.2.2.10.26. 2.2.10.26 Mercaptans
3.2.2.10.27. 2.2.10.27 Methylene Diamine (MDA)
3.2.2.10.28. 2.2.10.28 Nitriles
3.2.2.10.29. 2.2.10.29 O-Phenylenediamine (OPD)
3.2.2.10.30. 2.2.10.30 Phosphorus/phosphides
3.2.2.10.31. 2.2.10.31 Phthalates
3.2.2.10.32. 2.2.10.32 Polymers
3.2.2.10.33. 2.2.10.33 Resins
3.2.2.10.34. 2.2.10.34 Styrene
3.2.2.10.35. 2.2.10.35 Trimellitic Anhydride
3.2.2.10.36. 2.2.10.36 Triorthocresylphosphate (TOCP)
3.2.2.10.37. 2.2.10.37 Xylidine
3.2.2.11. 2.2.11 Syndromes Attributed to the Environment, Not Specified Elsewhere
3.2.2.11.1. 2.2.11.1 Event-Specific Syndromes (eg, Gulf War syndrome, World Trade Center cough)
3.2.2.11.2. 2.2.11.2 Mold
3.2.2.11.3. 2.2.11.3 Multiple Chemical Sensitivity Syndrome
3.2.2.11.4. 2.2.11.4 Tight Building Syndrome
3.3. 2.3 Natural Products
3.3.1. 2.3.1 Food Poisoning
3.3.1.1. 2.3.1.1 Bacterial
3.3.1.2. 2.3.1.2 Marine
3.3.2. 2.3.2 Fungi
3.3.2.1. 2.3.2.1 Mushrooms
3.3.2.2. 2.3.2.2 Other Fungal Toxins (eg, aflatoxins, trichothecene mycotoxins)
3.3.3. 2.3.3 Herbal and Dietary Supplements
3.3.4. 2.3.4 Plants
3.3.4.1. 2.3.4.1 Cardiovascular Toxic Plants (eg, Aconitum napellus,Nerium oleander)
3.3.4.2. 2.3.4.2 Cutaneous/Mucus Membrane Toxic Plants (eg, Toxicodendron
3.3.4.3. sp,Dieffenbachiasp)
3.3.4.4. 2.3.4.3 Gastrointestinal Toxic Plants (eg, Phytolacca Americana,
3.3.4.5. Solanumsp)
3.3.4.6. 2.3.4.4 Hepatotoxic Plants (eg, Bilghia sapida,Symphatumsp)
3.3.4.7. 2.3.4.5 Multisystem Toxic Plants (eg, Prunussp,Ricinus communis)
3.3.4.8. 2.3.4.6 Neurotoxic Plants (eg, Daturasp,Nicotiana tabacum)
3.3.5. 2.3.5 Toxic Envenomations
3.3.5.1. 2.3.5.1 Arthropods
3.3.5.2. 2.3.5.2 Marine Creatures
3.3.5.3. 2.3.5.3 Reptiles/Amphibians
3.4. 2.4 Warfare, Terrorism, and Riot Control Agents
3.4.1. 2.4.1 Biological
3.4.1.1. 2.4.1.1 Bacteria (eg, anthrax, plague)
3.4.1.2. 2.4.1.2 Toxins (eg, botulinum, staphylococcus B)
3.4.1.3. 2.4.1.3 Viruses (eg, smallpox)
3.4.2. 2.4.2 Chemical
3.4.2.1. 2.4.2.1 Acetylcholinesterase Inhibitors (eg, sarin, soman, VX)
3.4.2.2. 2.4.2.2 Blister Agents (eg, mustard)
3.4.2.3. 2.4.2.3 Incapacitating Agents (eg, calmatives, BZ [3-quinuclidinyl benzilate])
3.4.2.4. 2.4.2.4 Tear Gases (eg, pepper spray)
3.4.3. 2.4.3 Nuclear/Radiological
3.5. 3.0 Therapeutics
3.5.1. 3.1 ABCs: Resuscitation
3.5.2. 3.2 Initial Management
3.5.2.1. 3.2.1 Assessment Skills
3.5.2.1.1. 3.2.1.1 Differential Diagnosis
3.5.2.1.2. 3.2.1.2 Signs and Symptoms
3.5.2.1.3. 3.2.1.3 Toxidromes
3.5.2.2. 3.2.2 Decontamination Strategies
3.5.2.2.1. 3.2.2.1 Dermal
3.5.2.2.2. 3.2.2.2 Gastrointestinal
3.5.2.2.3. 3.2.2.3 Ocular
3.5.2.3. 3.2.3 Enhance Elimination Techniques
3.5.2.3.1. 3.2.3.1 Extracorporeal Removal
3.5.2.3.2. 3.2.3.2 Gastrointestinal Dialysis
3.5.2.3.3. 3.2.3.3 Urinary Approaches
3.5.3. 3.3 Pharmacological Basis of Antidote Use
3.5.3.1. 3.3.1 Antagonize Effects of Poison
3.5.3.1.1. 3.3.1.1 Enzyme Inhibitors (eg, physostigmine)
3.5.3.1.2. 3.3.1.2 Enzyme Reactivators (eg, pralidoxime)
3.5.3.1.3. 3.3.1.3 Physiological Antagonists (eg, calcium, glucagon)
3.5.3.1.4. 3.3.1.4 Receptor Antagonists (eg, atropine, flumazenil, naloxone)
3.5.3.1.5. 3.3.1.5 Reducing Agent (eg, methylene blue, N-acetylcysteine)
3.5.3.2. 3.3.2 Dispositional Agents
3.5.3.2.1. 3.3.2.1 Alcohol Dehydrogenase Antagonists
3.5.3.2.2. 3.3.2.2 Antivenoms/Antibodies
3.5.3.2.3. 3.3.2.3 Chelators
3.5.3.2.4. 3.3.2.4 Cyanide Antidotes
3.5.3.2.5. 3.3.2.5 Enzyme/Cofactor Replacement (eg, folinic acid, pyridoxine)
3.5.3.2.6. 3.3.2.6 Oxygen/Hyperbaric Oxygen
3.5.3.3. 3.3.3 Other Antidotes
3.5.4. 3.4 Supportive and Other Care
3.5.4.1. 3.4.1 Adjunctive Therapy (eg, granulocyte colony-stimulating factor)
3.5.4.2. 3.4.2 Anticonvulsants
3.5.4.3. 3.4.3 Antidysrhythmics
3.5.4.4. 3.4.4 Control of Agitation
3.5.4.5. 3.4.5 Control of Temperature
3.5.4.6. 3.4.6 Correct Electrolyte and Acid-Base Disturbances
3.5.4.7. 3.4.7 Critical Care Procedures (eg, arterial catheter and central line placement-
3.5.4.8. 3.4.8 Fluid Resuscitation
3.5.4.9. 3.4.9 Patient Monitoring
3.5.4.10. 3.4.10 Pressor Agents and Control of Blood Pressure
3.5.4.11. 3.4.11 Protect Airway/Ventilation/Manage Airway Injury
3.5.4.12. 3.4.12 Psychiatric Issues
3.5.4.13. 3.4.13 Social Issues
3.5.4.14. 3.4.14 Transplantation
3.5.5. 3.5 Withdrawal Syndrome Management
3.5.5.1. 3.5.1 Alcohol
3.5.5.2. 3.5.2 Opioid
3.5.5.3. 3.5.3 Sedative-Hypnotic
3.5.5.4. 3.5.4 Stimulant and Nicotine
3.5.5.5. 3.5.5 Mixed Pattern
3.6. 4.0 Assessment and Population Health
3.6.1. 4.1 Criteria for Causal Inference
3.6.1.1. 4.1.1 Biological Plausibility
3.6.1.2. 4.1.2 Consistency
3.6.1.3. 4.1.3 Dose-Response Relationship (biological gradient)
3.6.1.4. 4.1.4 Specificity (of exposure or outcome)
3.6.1.5. 4.1.5 Strength of Association
3.6.1.6. 4.1.6 Temporal Relationship
3.6.2. 4.2 Information
3.6.2.1. 4.2.1 Consultation Resources (eg, databases, National Library of Medicine)
3.6.2.2. 4.2.2 Surveys/Surveillance (eg, poison center data, National Report on Human Exposures
3.6.3. 4.3 Monitoring
3.6.3.1. 4.3.1 Biological Monitoring and Biomarkers (eg, population norms, indicators of excessive exposure)
3.6.3.2. 4.3.2 Environmental Sampling/Exposure Monitoring
3.6.4. 4.4 Occupational Assessment/Prevention
3.6.4.1. 4.4.1 Medical Surveillance
3.6.4.2. 4.4.2 Personal Protective Equipment
3.6.4.3. 4.4.3 Preemployment Screening
3.6.5. 4.4.4 Workplace Safety Engineering
3.6.6. 4.5 Principles of Epidemiology and Statistics
3.6.6.1. 4.5.1 Statistical Concepts (eg, interpretation of Pvalue, power calculation)
3.6.6.2. 4.5.2 Study Design
3.6.6.2.1. 4.5.2.1 Basic Types (eg, case series, randomized controlled trial)
3.6.6.2.2. 4.5.2.2 Basics of Validity/Generalizability (eg, bias, confounding, randomisation
3.6.6.2.3. 4.5.2.3 Measurements (eg, sensitivity, predictive value, limits of detection)
3.6.6.2.4. 4.5.2.4 Measures of Association (eg, odds ratios)
3.6.7. 4.6 Regional Poison Centers
3.6.7.1. 4.6.1 Administration/Organization
3.6.7.2. 4.6.2 Consultation at a Distance
3.6.7.3. 4.6.3 Education
3.6.7.4. 4.6.4 Prevention
3.6.7.5. 4.6.5 Surveillance/Interaction With Other Professional Health Organizations
3.6.7.6. 4.6.6 Triage
3.6.8. 4.7 Response to Hazardous Materials (Hazmat) Incidents, Including Terrorism
3.6.8.1. 4.7.1 Chemical Weapons Convention and Other Treaties
3.6.8.2. 4.7.2 Decontamination (eg, patients and responders)
3.6.8.3. 4.7.3 Incident Command System, Site Safety, and Control Zones
3.6.8.4. 4.7.4 Incident Response Planning and Emergency Preparedness
3.6.8.5. 4.7.5 National Pharmaceutical Stockpile: Deployment
3.6.8.6. 4.7.6 National Response Team: Federal Agency Coordination
3.6.8.7. 4.7.7 Regulatory and Legal Background (eg, Hazardous Waste Operations
3.6.9. 4.8 Risk
3.6.9.1. 4.8.1 Risk Assessment
3.6.9.1.1. 4.8.1.1 Carcinogenicity Testing
3.6.9.1.2. 4.8.1.2 Extrapolation From High to Low Dose
3.6.9.1.3. 4.8.1.3 Extrapolation of Animal Studies to Humans
3.6.9.1.4. 4.8.1.4 Human Epidemiological Studies in Risk Assessment
3.6.9.1.5. 4.8.1.5 Interpretation of Key Terms (eg, recommended exposure limit [REL])
3.6.9.1.6. 4.8.1.6 No Observed and Lowest Observed Adverse Effect Levels (NOAEL, LOAEL)
3.6.9.1.7. 4.8.1.7 Role of Risk Assessment in Formulating Regulations
3.6.9.1.8. 4.8.1.8 Target Risks (eg, 10 or 10 )
3.6.9.1.9. 4.8.1.9 “Uncertainty Factors” (reasons for them, approximate values)
3.6.9.2. 4.8.2 Risk Perception and Risk Communication
3.6.10. 4.9 Role of Federal and International Agencies in Toxicology
3.6.10.1. 4.9.1 Agency for Toxic Substances and Disease Registry (ATSDR)
3.6.10.2. 4.9.2 Centers for Disease Control and Prevention (CDC)
3.6.10.3. 4.9.3 Consumer Product Safety Commission (CPSC)
3.6.10.4. 4.9.4 Environmental Protection Agency (EPA)
3.6.10.5. 4.9.5 Food and Drug Administration (FDA)
3.6.10.6. 4.9.6 Health Resources and Services Administration (HRSA)
3.6.10.7. 4.9.7 National Institute of Occupational Safety and Health (NIOSH)
3.6.10.8. 4.9.8 Occupational Safety and Health Administration (OSHA)
3.6.10.9. 4.9.9 World Health Organization (WHO)
3.6.11. 4.10 Toxic Outbreaks of Historical Significance (eg, yusho, toxic oil)
3.7. 5.0 Analytical and Forensic Toxicology
3.7.1. 5.1 Assay Methods and Interpretation
3.7.1.1. 5.1.1 Clinical Drug Testing
3.7.1.1.1. 5.1.1.1 Confirmatory Tests
3.7.1.1.2. 5.1.1.2 Screening Tests
3.7.1.1.3. 5.1.1.3 Serum/Blood Drug Levels and Interpretation
3.7.1.1.4. 5.1.1.4 Urine Drug Testing
3.7.1.2. 5.1.2 Hair Analysis
3.7.1.3. 5.1.3 Laboratory Issues
3.7.1.3.1. 5.1.3.1 Point of Care Testing
3.7.1.3.2. 5.1.3.2 Quality Assurance/Quality Control
3.7.1.4. 5.1.4 Special Toxicology Testing
3.7.1.4.1. 5.1.4.1 Heavy Metal Screens
3.7.1.4.2. 5.1.4.2 Cholinesterase Determinations
3.7.1.5. 5.1.5 Therapeutic Drug Monitoring
3.7.2. 5.2 Laboratory and Other Diagnostic Assessments
3.7.2.1. 5.2.1 Anion Gap
3.7.2.2. 5.2.2 Blood Gases and Co-oximetry
3.7.2.3. 5.2.3 Electrolytes
3.7.2.4. 5.2.4 Hematologic and Coagulation Abnormalities
3.7.2.5. 5.2.5 Liver Function Tests
3.7.2.6. 5.2.6 Osmolality
3.7.2.7. 5.2.7 Renal Manifestations (eg, urine color, crystals)
3.7.2.8. 5.2.8 Other Supportive Testing
3.7.2.8.1. 5.2.8.2 Electroencephalography
3.7.2.8.2. 5.2.8.1 Diagnostic Imaging
3.7.2.8.3. 5.2.8.3 Electrocardiography
3.7.2.8.4. 5.2.8.4 Electromyography/Nerve Conduction Studies
3.7.3. 5.3 Forensics
3.7.3.1. 5.3.1 Chain of Custody
3.7.3.2. 5.3.2 Clandestine Laboratories
3.7.3.3. 5.3.3 Definition and Scheduling of Controlled Substances
3.7.3.4. 5.3.4 Interpretation of Postmortem Drug Levels
3.7.3.5. 5.3.5 Necrokinetics
3.7.3.6. 5.3.6 Selection of Postmortem Specimens
3.7.3.7. 5.3.7 Special Issues
3.7.3.7.1. 5.3.7.1 Meconium
3.7.3.7.2. 5.3.7.2 Vitreous Humor
3.7.4. 5.4 Legal Ethanol
3.7.4.1. 5.4.1 Alcohol and the Law
3.7.4.2. 5.4.2 Alcohol-Induced Psychomotor Impairment
3.7.4.3. 5.4.3 Blood and Urine Alcohol Analysis
3.7.4.4. 5.4.4 Breath Alcohol Analysis
3.7.4.5. 5.4.5 Collection and Storage of Alcohol Specimens
3.7.4.6. 5.4.6 Disposition of Alcohol
3.7.4.7. 5.4.7 Saliva and Other Media
3.7.5. 5.5 Medical Legal Issues (eg, role of expert witness)
3.7.6. 5.6 Workplace Drug Test Interpretation
3.7.6.1. 5.6.1 Cutoffs
3.7.6.2. 5.6.2 Guidelines for Federal Workplace Drug Testing Programs
3.7.6.3. 5.6.3 Role of Medical Review Officer (MRO)
4. Aims
4.1. An outline of a core curriculum for clinical toxicology
4.1.1. High standard
4.1.1.1. Evidence based
4.1.1.2. Experienced base
4.1.2. Free
4.1.3. Flexible to reflect change
4.2. The identification of which elements of this curriculum would be suitable for specific audiences
4.3. The support of this curriculum with “open source” teaching materials
4.4. A mechanism for gathering, assessing and distributing such material
4.5. This proposal is not specifically looking at accreditation of clinical toxicology training
5. Delivery Structures
5.1. Structures
5.1.1. Non website
5.1.1.1. Books
5.1.1.2. CD rom
5.1.2. Web based
5.1.2.1. Fixed
5.1.2.1.1. Website
5.1.2.1.2. Blackboard
5.1.2.2. Wiki
5.1.2.2.1. Plus
5.1.2.2.2. Minus
5.1.2.2.3. Proposal
5.2. Models
5.2.1. Course material with no accreditation
5.2.1.1. Plus
5.2.1.1.1. Variable output
5.2.1.1.2. Multiple Providers
5.2.1.1.3. Allows extraction of content for local audience
5.2.1.2. Minus
5.2.1.2.1. No WHO status
5.2.2. Course material with Accreditation
5.2.2.1. Plus
5.2.2.1.1. Status
5.2.2.2. Minus
5.2.2.2.1. labour intensive
5.2.2.2.2. Centralised
5.2.2.2.3. Difficult to taylor to specific audiences
5.2.2.2.4. Loss of ownership
5.2.2.2.5. Reduction of input
6. Funding
6.1. WHO
6.2. Donations
7. Target Audience
7.1. Direct
7.1.1. Poisons Information Specialists
7.1.2. Nurses
7.1.3. Doctors
7.1.4. Undergraduate
7.1.5. Postgraduate
7.2. Indirect
7.2.1. Filtered thru a local provider
7.2.1.1. Hospitals
7.2.1.1.1. Nurses
7.2.1.1.2. Doctors
7.2.1.2. Universities
7.2.1.2.1. Undergraduate
7.2.1.2.2. Postgraduate
7.2.1.3. Poisons Information Service
7.2.1.3.1. Poisons Information Specialists
8. Contribution
8.1. Quality
8.2. Sources of material
8.3. Acknowledging contributions
8.4. Conflict Resolution
8.4.1. Sources of Conflict
8.4.1.1. Inevitable Intellectual debate
8.4.1.2. Resource determined
8.4.2. How much can we tolerate?
8.4.3. Is conflict important to resolve?
8.4.4. Should we be paralysed by consensus?
8.4.5. Editorial mechanisms
8.5. Copyright
8.5.1. No Copyright
8.5.2. Copyright in Commons
8.5.2.1. Welcome | Creative Commons
8.5.2.2. Microsoft Addin
8.5.2.2.1. Download details: Office Add-in: Creative Commons Add-in for Microsoft Office
8.5.2.2.2. Also and Openoffice addin
8.5.2.3. Welcome | Science Commons
8.5.2.4. Documents
9. Content Description
9.1. Should we stratify curriculum outline?
9.1.1. Audience and Geography
9.1.2. Teaching Opportunity
9.2. Should we stratify content?
9.3. Curriculum topic
9.3.1. Monograph
9.3.1.1. Linked resources
