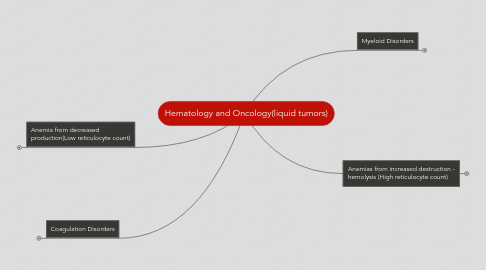
1. Anemia from decreased production(Low reticulocyte count)
1.1. Microcytic Anemias
1.1.1. Iron Deficiency
1.1.1.1. Pathology/Etiology- Loss of iron needed for heme production in erythrocytes. Women lose iron during menses, pregnancy, lactation, or occult hemorrhage. Men lose iron from occult hemorrhage, almost always from the GI tract. Iron deficiency anemia in men and post-menopausal women requires a work-up to exclude GI malignancy.
1.1.1.2. Presentation- Weakness, fatigue, lightheadedness, tachycardia, shortness of breath, or worsening of angina(chest pain). “PICA” symptoms – unusual cravings to chew dirt, clay, or ice(most common). Cells are small (low MCV) from decreased amount of hemoglobin per cell. The reticulocyte count is low since erythrocytes are produced in lower numbers. Ferritin (the storage form of iron) is usually the best indicator of iron storage levels. A high total iron binding capacity and a low serum iron level is another indicator iron deficiency
1.1.1.3. Treatment- Oral iron is the treatment of choice. Intravenous iron can be given in select situations.
1.1.2. Thalassemia
1.1.2.1. Pathology/Etiology- Mutations in either the alpha or beta globin chain resulting in decreased production of hemoglobin(Hb), and subsequently decreased erythrocyte production. Thalassemia is more common in people of Southeast Asian, African, or Mediterranean descent.
1.1.2.2. Presentation- Very wide spectrum of presentation, as it can be mild and asymptomatic, or can be very severe and life threatening. In severe thalassemia, symptoms include weakness, fatigue, lightheadedness, tachycardia, and shortness of breath – evident after six months of life. In most cases, low MCV with a low reticulocyte count. In beta thalassemia there is increased percentage of Hb A2 (α2σ2) on Hb electrophoresis, due to the decreased amount of Hb A(there is actually NOT an increase in the amount of Hb A2 produced!!!). Definitive diagnosis of alpha-thalassemia requires DNA analysis.
1.1.2.3. Treatment- If severe anemia, then will require transfusion. Eventually iron chelation for iron overload from multiple transfusions will be required for the severe cases. Allogeneic bone marrow transplantation can be curative – but extremely risky. For mild cases, no treatment is necessary.
1.1.3. Anemia of Inflammation
1.1.3.1. Pathology/Etiology- Inflammation stimulates hepcidin production, which shuts down iron transport. Therefore, iron sequestered in macrophages, and is not available for red cell production
1.1.3.2. Presentation- Typically, the underlying inflammatory condition(ie, infection, rheumatoid arthritis, etc) causes the symptoms. Though patients may be more fatigued from low red count. Will causes microcytosis eventually, but in early stages, may have normocytic anemia.
1.1.3.3. Treatment- Treat the underlying illness.
1.1.4. Other microcytic anemias, include Lead toxicity, and congenital sideroblastic anemias
1.2. Macrocytic Anemias
1.2.1. Folate/B12 Deficiency
1.2.1.1. Pathology- Loss of folate and/or B12 leads to decreased DNA synthesis in all hematopoietic cells. Therefore, granulocytes and platelets can also be decreased, not just erythrocytes. Neurons affected in B12 deficiency (NOT in folate deficiency). Folate is in green vegetables, so that deficiency most commonly results from poor diet (alcoholics, anorexia/bulemia), while B12 deficiency is typically in animal protein, so it results from acquired poor absorption (loss of intrinsic factor in pernicious anemia, gastric bypass surgery, or GI damage as in sprue or Crohn’s disease) or in people who are strict vegans. Occurs equally in men or women.
1.2.1.2. Presentation- Symptoms include weakness, fatigue, lightheadedness, tachycardia, and shortness of breath. Also, depression, peripheral neuropathy and abnormal balance may be present in B12 deficiency (NOT folate deficiency). Since the erythrocytes are blocked from dividing, they tend to be abnormally large (high MCV). The reticulocyte count is still low since erythrocytes are released into the circulation in reduced numbers.
1.2.1.3. Treatment- Oral folate for folate deficiency. Since the majority of B12 deficiencies are due to poor GI absorption, parenteral B12 is most often given. Note, if a patient is B12 deficient, and the patient is given folate, it can make the neurologic symptoms worse(since folate is not involved in this pathway, it will grab the B12, and direct to production of hematopoietic cells)
1.2.2. Other causes of Macrocytic anemias include myelodysplastic syndromes(see Myeloid lecture), medications (such as chemotherapy drugs), hypothyroidism, and liver disease
1.3. Normocytic anemias
1.3.1. Low erythropoietin states (e.g. renal disease), aplastic anemia, bone marrow infiltration (such as multiple myeloma), infection (such as Parvovirus B19 or HIV), medications.
2. Coagulation Disorders
2.1. Bleeding Disorders
2.1.1. INHERITED CONDITIONS
2.1.1.1. Hemophilia
2.1.1.1.1. Pathology - X-linked recessive trait. ~1/3 are spontaneous mutations -Mutations in the Factor VIII gene cause Hemophilia A (85% of hemophilias) – 1/5000-1/10,000 male births - Mutations in the Factor IX gene = Hemophilia B (12% of hemophilias) – 1/30,000 male births - The mutations lead to reduced production of the factor Severe Deficiency < 1% of normal factor levels Moderate Deficiency 1-5% of normal factor levels Mild Deficiency 5-15% of normal factor levels
2.1.1.1.2. Presentation- Bleeding into joints (hemarthroses) or large muscles. Normal Protime(PT), while the activated partial thromboplastin time (aPTT) is prolonged. The aPTT corrects with the addition of normal plasma(mixing study), indicating a factor deficiency as opposed to an inhibitor. Individual clotting factor levels are then assayed.
2.1.1.1.3. Treatment- Replacement with either recombinant or detergent-treated specific factor as soon as possible upon hemorrhage. Pre-treatment with factor prior to any surgical or dental procedure.
2.1.1.2. Von Willibrand’s Disease – Most common inherited bleeding condition
2.1.1.2.1. Pathology- Mutations in the Von Willibrand’s gene cause either quantitative or qualitative defects of VWF. These defects lead to decreased platelet adhesion and/or decreased Factor VIII levels (VWF carries FVIII in blood). Three types VWD i. Type 1 – Mild to moderate deficiency (autosomal dominant inheritance) ii. Type 2 – Functional Defect (4 subtypes – most of which are autosomal dominant) iii. Type 3 – Absolute deficiency (autosomal recessive trait)
2.1.1.2.2. Presentation- Bleeding from mucosal surfaces, menorrhagia, bleeding after minor procedures (commonly dental procedures). Usually, has a prolonged aPTT, which would correct with a mixing study. Normal PT.
2.1.1.2.3. Treatment- Desmopressin will stimulate release of VWF in some subtypes. The other subtypes require replacement with concentrates of VWF and FVIII.
2.1.2. ACQUIRED CONDITIONS
2.1.2.1. Vitamin K deficiency
2.1.2.1.1. Pathology – Reduction in the levels of the Vitamin K dependent factors (II, VII, IX, X). Results from a lack of intake of foods rich with Vitamin K (green leafy vegetables), a fat soluble vitamin, or from antibiotics, which will eliminate the gut flora, which is a source of Vitamin K. A functional vitamin K deficiency results from the use of warfarin or the intake of an ingredient in rat poison, brodifacoum.
2.1.2.1.2. Presentation – Easy bruising, hematuria, nosebleeds. Prolongs both PT and PTT. Will correct with a mixing study.
2.1.2.1.3. Treatment – Vitamin K supplements, which will take 8-12 hours to work or Factor concentrates or Fresh Frozen plasma (FFP), which work immediately.
2.1.2.2. Factor Inhibitors
2.1.2.2.1. Pathology – Autoantibody (typically IgG) against a specific factor, which inhibits that factor’s function. The most common factor affected is Factor VIII. *i.e. Lupus Anticoagulant
2.1.2.2.2. Presentation- Increased bruising, hematuria, joint bleeds, muscle bleeds. The PT or PTT(or both) will be prolonged based on which factor is being inhibited (for example, an inhibitor against FVIII will only cause the PTT to be prolonged, the PT will be normal). The prolonged clotting time will not correct with the addition of normal plasma (mixing study), because the inhibitor will bind and inactivate the factor in the normal plasma as well.
2.1.2.2.3. Treatment- Immunosuppression with steroids or other agents to reduce production of the autoantibody. Recombinant FVIIa can bypass the inhibitor in many cases.
2.2. Platelet Disorders
2.2.1. INHERITED CONDITIONS – these are very rare conditions
2.2.1.1. Glanzmann’s Thrombasthenia
2.2.1.1.1. Pathology- Congenital lack of Glycoprotein IIb/IIIa on platelet membrane leads to lack of platelet aggregation.
2.2.1.1.2. Presentation- Petechiae, nose bleeds, conjunctival hemorrhage. Normal PT and PTT.
2.2.1.1.3. Treatment- Platelet transfusions are used.
2.2.1.2. Bernard-Soulier
2.2.1.2.1. Congenital lack of Glycoprotein Ib on platelet membrane leads to lack of platelet adhesion.
2.2.1.2.2. Presentation- Petechiae, nose bleeds, conjunctival hemorrhage. Normal PT and PTT.
2.2.1.2.3. Treatment- Platelet transfusions are used.
2.2.1.2.4. Large MPV because platelets are large.
2.2.1.3. Wiskcott Aldrich
2.2.1.3.1. Can have very small platelets MPV < 6 from birth. Children will have other symptoms but the low MPV from birth is pathomneumonic for Wiskcott Aldrich syndrome.
2.2.1.4. May-Hegglin
2.2.1.4.1. Description: May-Hegglin anomaly (MHA) is an autosomal dominant disorder characterized by various degrees of thrombocytopenia that may be associated with purpura and bleeding; giant platelets containing few granules; and large, well-defined, basophilic, cytoplasmic inclusion bodies in granulocytes that resemble Döhle bodies (see the image below).
2.2.1.4.2. Large MPV b/c platelets are large.
2.2.1.4.3. History: In 1909, May described the presence of leukocyte inclusions and large platelets in an asymptomatic young woman. In 1945, Hegglin described a man and his 2 sons who were healthy but had a triad consisting of thrombocytopenia, giant platelets, and leukocyte inclusions. This diagnostic triad was later given the eponym May-Hegglin anomaly (MHA). [2] MHA is an autosomal dominant disorder characterized by various degrees of thrombocytopenia that may be associated with purpura and bleeding; giant platelets containing few granules; and large (2-5 µm), well-defined, basophilic, cytoplasmic inclusion bodies in granulocytes that resemble Döhle bodies. [1] MHA is one of a family of macrothrombocytopenias characterized by mutations in the MYH9 gene. [3] The other members of this family include Sebastian syndrome, [4] Epstein syndrome, [5] and Fechtner syndrome. [6] Most patients with MHA do not have clinically significant problems with bleeding and therefore do not require treatment.
2.2.1.4.4. Pathophysiology: Patients with MHA have a mutation of the MYH9 gene present in chromosomal region 22q12-13. [7, 3] The mutation results in disordered production of nonmuscle myosin heavy-chain type IIA, which leads to invariable macrothrombocytopenia secondary to defective megakaryocyte maturation. [8] Platelet function in patients with MHA has been reported as normal. [9, 10] ; however, in one study, epinephrine response was described as abnormal in 8 of 15 patients. [11] Leukocyte Döhlelike inclusion bodies are visualized on standard Wright stain and appear bright blue and spindle-shaped. Ultrastructural studies reveal that these bodies consist of clusters of ribosomes oriented along parallel myosin heavy-chain filaments 7–10 nm in diameter. [12] Neutrophil function is considered to be normal, and patients have no increased susceptibility to infections.
2.2.2. ACQUIRED CONDITIONS
2.2.2.1. Immune Thrombocytopenia Purpura(ITP)
2.2.2.1.1. Pathology – Autoantibodies against platelets that leads to rapid consumption of the platelets. When it occurs in children, there is often a viral prodrome, and it is usually self-limiting. In adults, usually no viral prodrome, and can often become a chronic condition. Associated with infective agents(HIV and Hep C), medications and pregnancy.
2.2.2.1.2. Presentation- Petechiae, nose bleeds, conjunctival hemorrhage. Normal PT and PTT. May have markedly low platelet count (< 5,000/cumm). Can have a large MPV as the immune response toward the platelets are beginning to resolve. Remember the autoantibodies toward platelets are in both the periphery and in the bone marrow.
2.2.2.1.3. Treatment – Steroids to suppress the immune system. Can give intravenous immunoglobulin(IVIG) if need to bring up the platelet count quickly. Splenectomy is a 2nd line therapy.
2.2.2.2. Thrombotic Microangiopathies
2.2.2.3. Thrombotic Thrombocytopenia Purpura(TTP)
2.2.2.3.1. Pathology: Etiology related to the lack of ADAMTS-13 – a metalloproteinase that cleaves the ultra large Von Willebrand multimers to large VWF multimers. Associated with pregnancy and HIV.
2.2.2.3.2. Diagnosis - Clinical - Pentad (only found ~50% of time)- –Microangiopathic hemolytic anemia(MAHA) - CNS symptoms – 60 –70% –Renal dysfunction – 50% –Fever – 25 – 60% –Thrombocytopenia
2.2.2.3.3. Treatment - Plasma Exchange - has reduced mortality from > 90% to < 10%
2.2.2.4. Hemolytic Uremic Syndrome(HUS)
2.2.2.4.1. Typically, no deficiency in ADAMTS-13. More often endothelial damage precipitating cause. Infection – most common association, especially E. Coli O157:H7 and Shigella. Also, recently associated with certain complement deficiencies. Treatment o Supportive – ie, dialysis if needed o Role for plasma exchange is unclear o For Complement associated HUS - eculuzimab
2.2.2.5. Venous Thromboembolism(VTE)
2.2.2.5.1. Pathology These disorders predispose patients to thrombotic events by loss of inhibition of the coagulation cascade or by enhancing the coagulation system. Ultimately, related to Virchow’s Triad: Stasis, Abnormal vessel wall, Hypercoagulability of blood STASIS – things that slow the flow of blood - Prolonged immobility – eg, hospitalization, long plane flight ABNORMAL VESSEL WALL – damage to the wall of the vessel(seen with chemotherapy) or abnormal venous valves(associated with varicose veins) HYPERCOAGULABILITY of BLOOD
2.2.2.5.2. Inherited Hypercoagulable states
2.2.2.5.3. Diagnosis – Laboratory evaluation can be done for an inherited hypercoagulable condition or APLA in patients with unprovoked VTE •Do NOT check during an acute event as the protein C & S and antithrombin may be physiologically low during that time. Wait until off warfarin to check protein C & S as these are vitamin K dependent
2.2.2.5.4. Presentation- These patients present with unprovoked deep venous thromboses or pulmonary emboli, which are often recurrent. Women may also present with recurrent spontaneous abortions. If a patient has an unprovoked VTE, then there is a 40% chance of having another VTE in the next 5 years off of anticoagulation.
2.2.2.5.5. Treatment – Anticoagulation
2.2.2.6. Disseminated Intravascular Coagulation (DIC)
2.2.2.6.1. Definition: Abnormal activation of the coagulation system leading to excess thrombin formation (another more descriptive term is Consumptive Thrombohemorrhagic disorder). DIC always results from some other disease process, it does not occur spontaneously.
2.2.2.6.2. Pathology: In DIC, thrombin is abnormally activated, and subsequently consumes other pro- and anticoagulant proteins. Can present as clotting or bleeding (or both). Can be an acute process or can be chronic. Etiology 1) Infections (endotoxin mediated – exposure of free tissue factor) –Bacterial (eg., Meningococcus) 2) Malignancies (Expression of tissue factor/ blood vessel wall damage) –Solid tumors(eg, prostate cancer) –Acute Leukemias(Acute Promyelocytic Leukemia- increased fibrinolysis) 3) Tissue damage (release of tissue factor/ endothelial damage) –Trauma (especially brain injury) –Burns 4) Vascular disorders (Vessel injury/endothelial damage) –Aortic aneurysm 5) Immunologic disorders (cytokine release) –Acute hemolytic transfusion reactions -Anaphylaxis 6) Direct enzyme activation (direct activation of coagulation) –Snake venom 7) Obstetrical complications (exposure of tissue factor) –Amniotic fluid embolism –Retained dead fetus
2.2.2.6.3. Diagnosis – ultimately a clinical diagnosis, with support from laboratory analysis Screening tests –•Platelet count – Most sensitive, but not specific •D-Dimer – sensitive, not specific •Protime – elevated ~ 75% of the time •aPTT – elevated ~ 60% of the time •Fibrinogen -very specific – if no underlying liver disease. But not sensitive
2.2.2.6.4. Treatment - Ideally correct the underlying abnormality. Support patient with blood products if necessary (eg. If bleeding, FFP and platelets) or use anticoagulants if patient clotting.
3. Anemias from increased destruction - hemolysis (High reticulocyte count)
3.1. Immune Hemolytic Anemia
3.1.1. Pathology- Auto-antibodies to the red cells lead to an acquired hemolytic anemia, where the antibody deposition on the red blood cells shortens their survival.
3.1.2. Presentation- Symptoms include weakness, fatigue, lightheadedness, tachycardia, and shortness of breath. Also, jaundice may occur. The reticulocyte count is high, and the MCV is also often high (due to increased number of reticulocytes). LDH and indirect bilirubin are high, and haptoglobin is low. The direct Coomb’s test is positive.
3.1.2.1. Coombs Testing
3.1.3. Treatment- Prednisone, or if that fails, then splenectomy, are the treatments of choice.
3.2. Non-immune Hemolytic Anemia
3.2.1. Hemoglobinopathies – Example -- Sickle Cell Anemia Pathology- A mutation in the β globin chain results in an abnormal hemoglobin that will aggregate when the intracellular oxygen concentration is low. These aggregates cause red cells to “sickle”, which leads to intravascular occlusion from these sickled red cells, which then causes hypoxia and pain. 8% of the African-American population is heterozygous for Hb S, 0.25% is homozygous.
3.2.2. Presentation- Normocytic anemia with a high reticulocyte count. Hb S with some Hb F (higher Hb F results in less symptoms for these patients) on hemoglobin electrophoresis. Pain crises may cause abdominal pain (splenic infarction), chest pain and shortness of breath from acute chest syndrome, stroke or seizures, leg ulcers, priapism, and bone necrosis. Infections with encapsulated organisms such as pneumococcus. Sickling episodes may be precipitated by infection, trauma, stress, high altitude.
3.2.3. Treatment- Oxygen, opiod and non-steroidal analgesics, rapid treatment of any infection, standard transfusions, exchange transfusions, folate supplementation, vaccines for encapsulated bacteria. In young patients with severe cases, allogeneic bone marrow transplantation can be curative-but is associated with high likelihood of death or long term disability.
3.3. Red cell enzyme abnormalities – Example -Glucose-6-phosphate dehydrogenase deficiency
3.3.1. The most common inherited hemolytic anemia is glucose-6-phosphate dehydrogenase deficiency (Asian, Mediterranean or African descent). Lack of this enzyme leads inability of red cell to eliminate free radicals, which damage the red cell membrane, and hence shortens red cell survival. Typically, induced by free radical formation from infections or medications, but certain subtypes can manifest after ingestion of Fava beans.
3.4. Red cell membrane abnormalities- Example - Hereditary spherocytosis, paroxysmal nocturnal hemoglobinuria
3.4.1. Hereditary Spherocytosis
3.4.2. Paroxysmal nocturnal hemoglobinuria
3.5. Microangiopathic Hemolytic anemia- caused be intravascular destruction of red cells, e.g. Thrombotic thrombocytopenia purpura, hemolytic uremic syndrome
4. Myeloid Disorders
4.1. LEUKEMIA
4.1.1. Acute Myelogenous Leukemia(AML)
4.1.1.1. Epidemiology - Incidence – 2.5/100,000 people/year – Median age – 63 years – 80-90% of adult leukemias – Causes include ionizing radiation, organic solvents such as benzene, previous chemotherapy, history of myelodysplastic syndrome (MDS), and inherited disorders of DNA repair (Down’s, Fanconi’s anemia, Wiskott-Aldrich), though most cases do not have an identifiable precipitating cause
4.1.1.2. Pathology - Acute Leukemia is a cancer of the bone marrow progenitor cells (progenitors are immature marrow cells still capable of division). -Myeloblasts (immature myeloid cells) proliferate and are unable to mature into normal cells. - These blasts eventually overwhelm the bone marrow, suppressing normal hematopoiesis. Therefore, it leads to decreased red cell, platelet, and neutrophil production. -Classically, eight subtypes of AML (FAB classification system); however, more recently divided into more categories.
4.1.1.3. Pathology (cont'd): Numerous known chromosomal (cytogenetic) abnormalities- some even associated w/ good prognosis.
4.1.1.3.1. 15:17 translocation- found in APML (AML- M3) Acute Promyelocytic Leukemia) This subtype of AML has the best prognosis >70% long term survival.
4.1.1.3.2. 8;21 translocation (found in AML-M2) and inversion 16 (found in AML-M4Eo) also associated with better prognosis.
4.1.1.3.3. By definition acute leukemia must have a least 20% leukemic blasts in the bone marrow to be considered acute!
4.1.2. Myelodysplastic Syndrome (MDS)
4.1.2.1. Epidemiology - Disease of the elderly - Occurs in about 1 out of 500 persons between 60-75 - Most cases idiopathic, but known causes include ionizing radiation, organic solvents such as benzene, and previous chemotherapy – note these are the same as AML
4.1.2.2. Pathology - A clonal disorder characterized by ineffective and disordered hematopoiesis - Abnormal clone overwhelms the bone marrow, and suppresses normal maturation of the other cell lines resulting in reduced production of red cells, myeloid cells and platelets - Typically characterized by chromosomal(cytogenetic) abnormalities
4.1.2.3. Presentation - Bone marrow failure • Anemia – fatigue, weakness, shortness of breath • Thrombocytopenia – increased bruising and bleeding • Leukopenia/neutropenia – infections
4.1.2.4. Treatment - Non-curable disease except by allogeneic bone marrow transplantation(though not available in most patients due to their age) - Certain chemotherapy agents have been shown to be effective to lessen transfusion requirement (DOES not cure!) - Supportive care – such as transfusion of red blood cells or platelets
4.1.3. Chronic Myelogenous Leukemia
4.1.3.1. Epidemiology - Occurs in 1/100,000 people - Median age is 43, but can develop at any age
4.1.3.2. Pathology - Proliferation of maturing myeloid elements - Characterized by the Philadelphia Chromosome (9;22 translocation) – this translocation connects bcr and abl (known as the bcr-abl translocation) – Identifying this translocation makes the diagnosis! - This translocation permanently turns on a tyrosine kinase that induces proliferation of the abnormal stem cell clone - Typically, white cells, red cells and platelet counts are elevated - Will always progress at some point to AML (called the blast phase of CML) - this type of AML is not cured with conventional therapy
4.1.3.3. Presentation - Patients can be asymptomatic - Weakness, fatigue from high white count due to increase cytokine release
4.1.3.4. Treatment - Targeted therapy – eg, Imatinib- which is directed at the tyrosine kinase produced by the bcr-abl translocation – induces full remissions but too soon to tell its long term effects on the disease - Only established curative option is allogeneic bone marrow transplantation
4.1.4. Acute Lymphocytic Leukemia(ALL)
4.1.4.1. Epidemiology – Incidence 1-3/100,000/year – 3,000 new cases of ALL/year – Peak incidence at 2-3 years – Second peak after 80 years – 10-20% of adult leukemias, but 90% of childhood leukemias
4.1.4.2. Pathology - Acute Leukemia is by definition a cancer of bone marrow progenitor cells (progenitors are immature marrow cells still capable of division) - Lymphoblasts (immature lymphocytes) proliferate and are unable to mature into normal cells - These blasts eventually overwhelm the bone marrow, suppressing normal hematopoiesis – therefore decreases red cell, platelet, and neutrophil production - By definition acute leukemia must have at least 20% leukemic blasts in the bone marrow - Can be of T or B cell origin - Often associated with chromosomal (cytogenetic) abnormalities, including the Philadelphia chromosome (9;22 translocation). This particular translocation is associated with a very poor response to conventional treatments - Burkitt’s Leukemia/Lymphoma – associated with cytogenetic abnormality t(8;14) – often has a better prognosis. Known to be associated with both Epstein-Barr virus and HIV
4.1.4.3. Presentation - Bone marrow failure • Anemia – fatigue, weakness, shortness of breath • Thrombocytopenia – increased bruising and bleeding • Leukopenia/neutrapenia – infections - Enlarged lymph nodes and/or splenomegaly - Mediastinal mass - Neurologic complaints (headaches, double vision, swallowing difficulty, etc) from leukemia in the central nervous system
4.1.4.4. Treatment – Prolonged chemotherapy (up to 3 years) or bone marrow transplant is certain situations. For children the cure rate is over 70%. For adults the cure rate is quite poor.
4.1.5. Chronic Lymphocytic Leukemia(CLL)
4.1.5.1. Epidemiology - Disease of advancing age - Approximately 10,000 new cases per year
4.1.5.2. Pathology - Proliferation of mature lymphocytes in the bone marrow - Majority are of B-cell origin - Usually an indolent process - Does not convert to ALL
4.1.5.3. Presentation - Often found incidentally on routine blood work (patient asymptomatic) - Can present secondary to bone marrow failure • Anemia – fatigue, weakness, shortness of breath • Thrombocytopenia – increased bruising and bleeding • Neutropenia (lack of neutrophils) – infections - Lymphadenopathy/Splenomegaly - B symptoms (night sweats, weight loss, fever).
4.1.5.4. Treatment- Typically, no treatment is needed until cytopenias or symptoms develop
4.2. Myeloproliferative Disorders – clonal stem cell disorders associated with abnormal proliferation of mature myeloid elements
4.2.1. Polycythemia Vera
4.2.1.1. Epidemiology - Occurs in 1-3/100,000 people - Median age of diagnosis is 65
4.2.1.2. Pathology - Disorder causes elevated red cell count, though often platelet count and white count are elevated as well - High red cell count causes hyperviscosity, leading to decreased oxygen delivery, and therefore poor CNS function - Combination of high red cell count and high platelet count increases substantially the risk of thrombotic episode such as a stroke or heart attack - Can convert to AML – but rare - Associated with a genetic mutation in the Janus Kinase 2 gene – the JAK2 V617F mutation – in over 95% of patients. Identifying this gene in the context of erythrocytosis establishes the diagnosis
4.2.1.3. Presentation - Headaches, “ruddy” complexion, visual changes, neuro symptoms from hyperviscosity of elevated red count - Stroke or heart attack
4.2.1.4. Treatment - Phlebotomy for elevated red cells - Meds to control platelet count - Antiplatelet medications (eg, Aspirin) to reduce risk of thrombosis
4.2.2. Essential Thrombocytosis
4.2.2.1. Epidemiology - Less common than P.Vera - Average age of diagnosis is 60-65 - Up to 25% are less than age 40 - Occurs more frequently in women
4.2.2.2. Presentation - Often patients are asymptomatic and found on routine blood work - Thrombotic event – such as stroke or heart attack
4.2.2.3. Pathology - Clonal stem cell disorder that causes increase platelet production - High platelet count increases risk for thrombosis and/or bleeding complications - Very rarely transforms into AML - Can be associated with the JAK2 mutation( similar to P. Vera), but only found in 50% of ET patients
4.2.2.4. Treatment - Young patients can often be observed - If >60 or history of thrombotic event, then can use meds to control the count - Antiplatelet medications (eg, Aspirin)
4.3. LYMPHOMA
4.3.1. Non-Hodgkin’s Lymphoma(NHL)
4.3.1.1. Epidemiology - NHL is rapidly increasing in incidence in the U.S., with 50,000 new cases/yr and 20,000 deaths/yr. - Age and any immunodeficiency (including HIV) increase risk.
4.3.1.2. Pathology - Malignancy can occur at any stage of lymphocyte development in the lymph node
4.3.1.2.1. There are multiple histologic types with differing proliferation rates
4.3.1.3. Pathology (cont'd): - NHL usually starts in the lymph nodes (or other lymphoid tissue) and spreads both via the lymphatics and hematogenously(through the blood) to adjacent nodes, the spleen, liver and/or bone marrow - Stage I- single node region, Stage II- 2 or more nodal groups on the same side of the diaphragm, Stage III- nodes on both sides of the diaphragm involved, Stage IV- any extra-lymphatic involvement (e.g. liver, marrow).
4.3.1.4. Presentation - Lymphadenopathy - B symptoms (night sweats, weight loss, fever). These represent a worse prognosis, and are added to the staging - Can present in extra-nodal sites (like liver and brain)
4.3.1.5. Treatment - Depends on the type of lymphoma - Indolent lymphomas can be observed with no treatment if they are not causing symptoms - Can use radiation, chemotherapy, or a combination of the two - Can use autologous bone marrow transplant for certain types of relapsed lymphoma
4.3.2. Hodgkin’s Lymphoma or Disease (HD)
4.3.2.1. Epidemiology - HD is uncommon, 8,000 new cases/yr with 2,000 deaths/yr - Incidence demonstrates a bimodal distribution – peak ages 15-35 and second smaller peak after age 50
4.3.2.2. Pathology - The characteristic malignant cell is the CD30+ Reed-Sternberg cell, thought to be an antigen presenting cell in the lymph node - HD starts in the nodes and spreads predominantly via the lymphatics to adjacent nodes(unlike NHL, it does not spread through the blood) - Stage I- single node region, Stage II- 2 or more nodal groups on the same side of the diaphragm, Stage III- nodes on both sides of the diaphragm involved, Stage IV- any extra-lymphatic involvement (e.g. liver, marrow)
4.3.2.3. Presentation - Lymphadenopathy - B symptoms (night sweats, weight loss, fever). These represent a worse prognosis, and are added to the staging
4.3.2.4. Treatment - Typically very responsive to treatment, so have very good long term survival (Cure!) - Local radiation alone can be curative for stage I - Chemotherapy(+/- Radiation) for Stage II-IV - Radiation and/or chemotherapy can cure > 75% of all HD - If relapsed, autologous stem cell transplantation can cure up to 45% of those relapses.
4.4. Multiple Myeloma
4.4.1. most common type of plasma cell dyscrasia
4.4.1.1. cell dyscrasia: abnormal disorders state of the cell.
4.4.2. Epidemiology - 13,000 new cases/yr – due to very recent advancements in therapy, these patients are living longer. - Advancing age, males, African-American race, and radiation exposure associated with an increased risk.
4.4.3. Pathology - A malignancy of antibody-producing plasma cells. They typically produce a monoclonal antibody(sometimes called a paraprotein) that can suppress the production of the normal antibodies, leading to a condition called hypogammaglobulinemia - In myeloma, the monoclonal antibodies are typically IgG and IgA (not IgM), but can be just the light chain (kappa/lambda) as well - Myeloma can create lesions in cortical bone leading to hypercalcemia, fractures, and spinal cord compression - Antibody deposition, hypercalcemia, hyperuricemia all can lead renal insufficiency - Abnormal plasma cells release substance that suppress red cell production which leads to anemia - Myeloma cells typically stay in the marrow but may also produce malignant masses, called plasmactyomas that can be found anywhere in the body; not a curable disorder.
4.4.4. Presentation - Bone pain from lytic lesions or fractures - Weakness and light-headedness from anemia - Infection from hypogammaglobulinemia - Nausea and vomiting, edema from renal failure - Confusion from hypercalcemia
4.4.5. Treatment - Chemotherapy - Bisphosphonates – bone hardening medicine to prevent fractures - Autologous stem cell transplantation has been shown to improve survival - Novel agents such as Thalidomide and its analogue and drugs called proteasome inhibitors
4.5. Primary Amyloidosis
4.5.1. – there are different types of amyloidosis, but the most common is primary amyloidosis, where immunoglobulins bind together to form the amyloid protein that is deposited into tissues (kidney, GI tract, heart, liver, spleen, skin) to cause damage to the organ. Often seen with multiple myeloma, but can be seen without myeloma as well.
4.6. Waldenstrom’s Macroglobulinemia
4.6.1. Plasma cell dyscrasia associated with increased production of IgM - Does not cause bone destruction or renal failure - Increased amount of IgM can cause hyperviscosity – slow movement of blood that can lead to decreased CNS function from decrease oxygen delivery -Is similar to an indolent lymphoma
