1. Pathogenesis
1.1. Progressive deterioration of hyaline cartilage at ends of bones
1.1.1. Worsens slowly over time
1.1.1.1. May stabilize over time
1.1.1.2. Often occurs as alternating periods of deterioration and stabalization
1.1.2. Normally smooth surfaces become rough or disappear over time
1.2. Idiopathic
1.2.1. Localized
1.2.1.1. < 2 affected joints
1.2.2. General
1.2.2.1. > 3 affected joints
1.2.3. No identifiable cause
1.3. Secondary
1.3.1. Congenital
1.3.2. Traumatic
1.3.3. Neuropathic
2. Risk Factors
2.1. Daily stress applied to joints
2.2. Women
2.2.1. 2-3 times more likely than men to develop
2.3. Age
2.3.1. Reductions in cartilage volume, proteoglycan content, cartilage vascularization, and cartilage perfusion
2.3.2. Age alone is an insufficient cause of cartilage
2.4. Obesity
2.4.1. Increased load on weight bearing joints
2.4.1.1. Knees and hips most often affected
2.5. Trauma
2.5.1. Can develop even in absence of obvious trauma
2.5.2. Results in increased microtrauma
2.6. Genetics
2.6.1. Methylation on osteoarthritis susceptibility genes
2.6.2. Contributing factor of heritable developmental defects and skeletal anomalies that can cause congenital misalignment of joints
2.7. Reduced levels of sex hormones
2.7.1. Estrogen levels
2.7.1.1. Increasing HRT may reduce incidence of knee and hip arthritis
2.8. Muscle weakness or dysfunction
2.9. Repetitive use
2.9.1. Heavy labor, bending, lifting
2.9.2. Frequent squatting, kneeling, climbing
2.9.3. Joint injuries
2.10. Infection
2.11. Crystal deposition
2.12. Acromegaly
2.13. Previous history inflammatory arthritis
2.13.1. Rheumatoid arthritis
2.13.2. Hand arthritis predisposes to knee arthritis
2.14. Heritable metabolic causes
2.14.1. Wilson disease
2.14.2. Hemochromatosis
2.15. Underlying morphologic risk factors
2.15.1. Congenital hip dislocation and slipped femoral capital epiphysis
2.15.2. Knee or hip malalignment
2.15.3. Scoliosis
2.16. Disorders of bone
2.16.1. Paget disease
2.16.2. Avascular necrosis
2.16.3. Osteoporosis
2.17. Previous surgical procedures
3. Incidence & Prevalence
3.1. Most common type of joint disease
3.1.1. More than 80-90% of people over 65 meet radiographic criteria for diagnosis
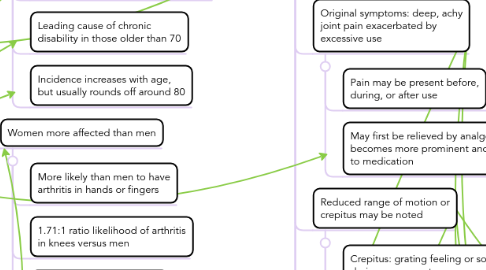
3.1.2. Leading cause of chronic disability in those older than 70
3.1.3. Incidence increases with age, but usually rounds off around 80
3.2. Women more affected than men
3.2.1. More likely than men to have arthritis in hands or fingers
3.2.2. 1.71:1 ratio likelihood of arthritis in knees versus men
3.2.3. 12:1 ratio likelihood of developing erosive arthritis versus men
3.3. Prevalence higher in Native Americans
3.3.1. Asians at lowest risk
3.4. More than 20 million affected people in the United States
3.4.1. Estimated cost over $100 million each year
3.4.1.1. Direct costs: clinical visits, medication, surgical intervention
3.4.1.1.1. Average $2600 per year per person
3.4.1.2. Indirect costs: loss of time at work
3.4.1.2.1. Average 13 days of lost work per year
3.4.1.2.2. $3.4-13.4 billion per year total in lost income
4. Clinical Manifestations
4.1. Slow progression of symptoms over years or decades
4.1.1. Usually presents after age 40
4.2. Original symptoms: deep, achy joint pain exacerbated by excessive use
4.2.1. Pain may be present before, during, or after use
4.2.2. May first be relieved by analgesics but eventually becomes more prominent and may not respond to medication
4.3. Reduced range of motion or crepitus may be noted
4.3.1. Crepitus: grating feeling or sound during movement
4.3.2. Possible relation to bone spurs [osteophytes]
4.3.2.1. Bony spurs: bony protuberances felt under skin near joint, growing over time
4.4. Stiffness at rest lasting at least 30 minutes
4.4.1. Occurring in the mornings or after periods of inactivity
4.4.2. May correspond with weather changes
4.5. Tenderness when pressure is applied
4.5.1. Pain levels are usually consistent over time
4.6. Weakness
4.7. Inflammation
4.7.1. Effusion caused by accumulation of excess fluid
4.8. Gait may be affected if weight bearing joints are afflicted
5. Diagnostics
5.1. Diagnostic testing
5.1.1. Plain radiography
5.1.1.1. Cost effective
5.1.1.2. Readily available and quickly obtained
5.1.1.3. Used for detection of joint space loss in high-load areas
5.1.2. CT scan
5.1.2.1. Rarely used
5.1.2.2. Often used to diagnose malalignment of patellofemoral joint or food and ankle joints
5.1.3. MRI
5.1.3.1. Rarely used
5.1.3.2. Detects joint narrowing, subchondral osseous changes, osteophytes
5.1.3.3. Direct visualization of articular cartilage and other joint tissues
5.1.4. Bone scanning
5.1.4.1. Used to differentiate from osteomyelitis or bone metastasis
5.1.4.2. Useful in early diagnosis of arthritis in hands
5.1.4.3. Results yield a symmetrically patterned, mildly increased uptake
5.1.4.4. Negative results may indicate multiple myeloma
5.1.5. Anthrocentesis
5.1.5.1. Diagnostic joint aspiration for synovial fluid analysis
5.1.5.2. Looking for presence of noninflammatory joint fluid
5.1.5.3. Can be used to exclude inflammatory arthritis, infection, or crystal arthropathy
5.2. When differentiating from rheumatoid arthritis, RA typically has the following manifestations but OA typically does not
5.2.1. Elevated WBC count
5.2.2. Inflammatory joint fluid
5.2.2.1. Polymorphonuclear leukocytes
5.2.3. Systemic inflammation
5.2.3.1. Elevated erythrocyte sedimentation rate
5.2.3.2. C-reactive protein levels
5.2.4. Positive serologies
5.2.4.1. Rheumatoid factors
5.2.4.2. Anti-cyclic citrullinated peptide antibodies
6. Treatment
6.1. Goals
6.1.1. Alleviation of pain
6.1.2. Improvement of functional status
6.2. Non-pharmocological treatments
6.2.1. Heat and cold
6.2.2. Weight loss
6.2.2.1. Loss of excess weight can slow cartilage loss on weight-bearing joints
6.2.3. Exercise
6.2.3.1. Cardiovascular or resistance training exercise for hips and knees
6.2.3.2. Aquatic exercise for hips and knees
6.2.3.3. Long-distance walking and resistance training programs
6.2.3.3.1. Helps slow functional decline
6.2.4. Occupational therapy
6.2.4.1. Joint protection techniques
6.2.4.2. Energy conservation techniques
6.2.4.3. ADL re-training
6.2.5. Physical therapy
6.2.5.1. Providing walking aids [assistive devices]
6.2.6. Assistive devices
6.2.6.1. May assist in over-exertion, pain management, or maintaining independence
6.2.6.2. Braces, splints, or appropriate footwear
6.2.6.3. Canes or walkers
6.2.7. Acupuncture
6.2.7.1. Pain relief
6.2.8. Pulse electromagnetic field stimulation
6.2.8.1. Pain relief
6.2.8.2. Maintaining proteoglycan composition of chondrocytes through downregulation of its turnover
6.3. Medication
6.3.1. Analgesics
6.3.1.1. Relief of mild to moderate pain
6.3.1.2. Acetaminophen
6.3.1.2.1. Drug of choice for patients who have a documented hypersensitivity to asprin or NSAIDs, a history of upper GI tract disease, or who are on anticoagulants
6.3.2. Topical analgesics
6.3.2.1. Used for superficial joints, like knees or hands
6.3.2.2. Capsaicin
6.3.2.2.1. Deletes substance P in peripheral sensory neurons
6.3.3. Opioid analgesics
6.3.3.1. Drug of choice for advanced patients who do not want, are too ill for, are not candidates for, or are trying to buy time for joint replacement surgery
6.3.3.2. Increases risks of falls and fall-related fractures, especially in the elderly
6.3.3.3. Tramadol
6.3.3.3.1. Alters perception of and response to pain, inhibits serotonin and norepinephrine reuptake
6.3.3.4. Oxycodone
6.3.3.4.1. Eventually replaced with a long-acting medication
6.3.4. NSAIDs
6.3.4.1. Analgesic, anti-inflammatory, antipyretic medication
6.3.4.2. Ketoprofin
6.3.4.2.1. Mild to moderate pain and inflammation relief
6.3.4.3. Piroxicam
6.3.4.3.1. Decreases formation of inflammatory mediators
6.3.4.4. Ibuprofen
6.3.4.4.1. Relieves mild to moderate pain and inflammation
6.3.4.5. Meloxicam
6.3.4.5.1. Decreases formation of inflammatory mediators
6.3.4.6. Diclofenac
6.3.4.6.1. Anti-inflammatory and analgesic properties
6.3.4.7. Naproxem
6.3.4.7.1. For mild to moderate pain, inhibits inflammatory reactions and pain
6.3.5. Antidepressants
6.3.5.1. Duloxetine
6.3.5.1.1. Used for chronic muscoloskeletal pain including discomfort from osteoarthritis and lower back pain
6.3.6. Corticosteroid injections
6.3.6.1. Triamcinolone, Betamethasone, Methylprednisolone
6.3.6.1.1. Reverses capillary permeability to decrease inflammation
6.3.6.2. Betamethasone
6.3.7. Antirrheumatic injections
6.3.7.1. Used to treat patients with osteoarthritic knee pain that is unresponsive to conservative nonpharmacologic therapy and simple analgesics
6.3.7.2. Sodium hyaluronate
6.3.7.2.1. Supports lubricating and shock-absorbing properties of articular cartilage
6.3.8. Skeletal muscle relaxants
6.3.8.1. No officially studied long-term results
6.3.8.2. Carisoprodol
6.3.8.2.1. Short acting, depressant effect at spinal level
6.3.8.3. Dantrolene
6.3.8.3.1. Reduces painful cramping and detrimental muscle tightening by reducing muscle action potential at muscle level
6.3.8.4. Baclofen
6.3.8.4.1. Central muscle relaxant that lessens flexor spasticity and hyperactive stretch reflexes of upper motor neurons
