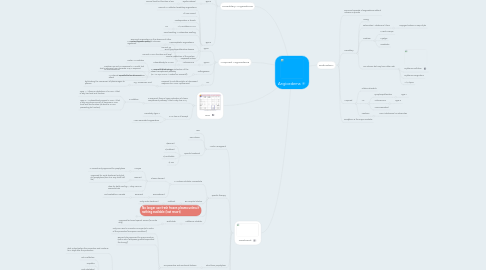
1. Hereditary Angioedema
1.1. C1 inhibitor gene
1.1.1. Serping 1 gene
1.1.1.1. Serine protease inhibitor
1.1.1.1.1. similar to angiotensin converting enzyme and alpha anti-tripsin
1.1.1.1.2. Site where it acts on
1.1.1.2. AD (25% de novo)
1.1.1.2.1. C1 estrase inhibitor low in both level and function
1.2. Type 1
1.2.1. Decrease production
1.3. Type 2
1.3.1. Dysfuncational
1.3.1.1. Normal level but function is low
1.4. Type 3
1.4.1. Normal C1 inhibitor hereditary angioedema
1.4.2. All invx normal
1.4.3. Predisposition in female
1.4.4. A/W mutation in FXII
1.4.4.1. AD
1.4.5. Facial swelling > extremities swelling
1.4.6. Proposed criteria
1.4.6.1. Recurrent angioedema in the absence of other cause (diseases, meds )
1.4.6.2. Normal C4
1.4.6.3. Normal C1INH function and level
1.4.6.4. One of the following
1.4.6.4.1. Factor XII mutation
1.4.6.4.2. Positive FHx and no response to 1 month trial of anti-histamines
1.4.6.4.3. An interval expected to be a/w 3 or more attack
2. Acquired Angioedema
2.1. Type 1
2.1.1. Paraneoplastic angioedema
2.1.1.1. Monoclonal gammopathy of unknown significant
2.1.2. B-cell lymphoproliferative disease
2.1.3. Due to catabolism of the protein
2.2. Type 2
2.2.1. Autoimmune
2.2.1.1. Autoantibody to C1INH
2.3. Pathogenesis
2.3.1. In acquired, there is hyper activation of the classic complement pathway (IC-->C1q,C1r,C1s-->C4b2a[C3 converts])
2.3.1.1. That is why you have decrease C1q in acquired.
2.3.1.2. C4 will also be decreased
2.4. Rx.
2.4.1. Respond to anti-fibrinolytic w/ decreased response to C1INH replacement
2.4.1.1. e.g. Tranexmeic acid
2.4.1.1.1. by blocking the conversion of plasminogen to plasmin
3. Invx
3.1. In acquired, there is hyper activation of classic complement pathway-->that is why low C1q
3.1.1. In addition
3.1.1.1. Type 1 -->there is catabolism of C1INH-->that is why low level and function
3.1.1.2. Type 2--->autoantibody against C1INH-->that is why may have normal or decrease C1INH level and low function (ab bind to C1INH preventing its function).
3.2. C4 is low in all except
3.2.1. Herediatry type 3
3.2.2. ACEI associated angioedema
4. Treatment
4.1. Acute Managment
4.1.1. ABC
4.1.2. Pain relieve
4.1.3. Specific treatment
4.1.3.1. 1)Berinert
4.1.3.2. 2)Icatibant
4.1.3.3. 3) Ecallintide
4.1.3.4. 4) FFP
4.2. Specific therapy
4.2.1. C1 estrase inhibitor concentrate
4.2.1.1. Plasma derived
4.2.1.1.1. Cinryze
4.2.1.1.2. Berinert
4.2.1.1.3. dose for both 20U/kg IV. They come in 500units/vials
4.2.1.2. Recombinant
4.2.1.2.1. Ruconest
4.2.2. B2 receptor blocker
4.2.2.1. Icatibant
4.2.2.1.1. Only acute treatment
4.2.3. No longer use fresh frozen plasma unless if nothing available (last resort)
4.2.3.1. Issue with it also contain complement
4.2.4. Kallikerine inhibitor
4.2.4.1. Ecallintide
4.2.4.1.1. Approved but need special access (for acute only)
4.3. Short term prophylaxis
4.3.1. Pre-procedure and emotional distress
4.3.1.1. Only one used in Canada is Cinryze (w/in 24hrs of the procedure [European Guideline])
4.3.1.2. Berinert also approved for pre-procedure (within 6hrs [European guideline specified the timing])
4.3.1.3. Attenuated androgens
4.3.1.3.1. Danazol
4.3.1.4. Fresh Frozen Plasma (last resort)
4.4. Long term prophylaxis
4.4.1. Cinryze
4.4.1.1. evidance is high, recom strong
4.4.2. Danazol
4.4.2.1. caution in female
4.4.3. Tranexamic acid
4.4.3.1. moderate especially for peds
4.4.4. Rituximab
4.4.4.1. for acquired angioedema
4.5. Preventions
4.5.1. • Preventions: No ACE inhib, no estrogens, no stress
5. Definiation:
5.1. Recurrent episode of angioedema without urticaria or pruritis
5.2. Hereditary
5.2.1. Young
5.2.2. Extremities > abdominal >face
5.2.2.1. Laryngeal edema in 50% of pts
5.2.3. Prodrom
5.2.3.1. Muscle cramps
5.2.3.2. Myalgia
5.2.3.3. Headache
5.2.4. No urticaria but may have other rash
5.2.4.1. Erythema multiform
5.2.4.2. Erythema marginatum
5.2.4.3. A/W lupus
5.3. Acquired
5.3.1. Older induvidula
5.3.2. Ax.
5.3.2.1. Lymphorpoliferative
5.3.2.1.1. Type 1
5.3.2.2. Autoimmune
5.3.2.2.1. Type 2
5.3.2.3. ACEI associated
5.3.3. Features
5.3.3.1. Face >abdominal or extremities
