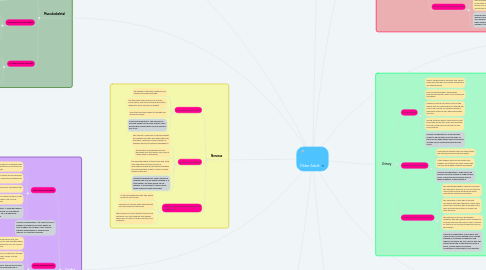
1. Cardiac
1.1. Heart rate may decrease
1.1.1. the SA node in the heart is considered the "pacemaker" of the heart and controls the pace the heart beats
1.1.2. over time fibrous tissue and fat deposits may form in the conduction pathways of the heart
1.1.3. The SA node looses cells throughout the aging process
1.1.4. all of the above cause the pace of the heart aka the heart rate to slow down/decrease
1.1.5. nursing considerations- a slight decrease in HR is normal and should occur gradually. Abrupt changes in HR or bradycardia should be reported.
1.2. nursing considerations- not everyone forms plaques and tangles, but older adults do have a higher risk of them. Don't assume patients with plaques or tangles have memory or cognitive problems.
1.3. weaker peripheal pulses
1.3.1. over time and after excessive use, the heart muscle begins to lose strength which decreases the contraction and can cause a lower cardiac output
1.3.2. since the blood isn't circulating as strongly in the hands and feet, pulses may be weaker in these areas
1.3.3. nursing considerations- the hands and feet may feel cool due to less blood flow. a slightly weaker peripheral pulse may be seen in older adults but pulses should still be present and equal bilaterally. Different medications can be prescribed such as digoxin to increase contractile strength and therefore increase peripheral blood flow. Palpate pulses when the patient is laying down with their feet in front of them. If they are sitting blood may pool at the feet due to gravity.
1.4. decrease in artery elasticity
1.4.1. arterial walls may stiffen, thicken, or both. Thickening of the artery walls from plaque build up is referred to as atherosclerosis. stiffening and thickening of artery walls is referred to as arteriosclerosis.
1.4.2. when the walls become stiff, thicker, or contain plaque build up the artery is less elastic and this can effect blood flow
1.4.3. if there is a build up or thicker artery walls the heart has to work harder to over come the resistance in the vessels to pass blood though. If the artery walls are also stiff then they cannot stretch to make the passage for blood wider. This causes increases in blood pressure.
1.4.4. high fat diets, smoking, and older age are the common reasons why people have decreased blood vessel elasticity
1.4.5. nursing considerations- blood thinners may be prescribe if there is a risk for a clot, antihypertensives may be prescribed if blood pressure rises, low fat diets should be encouraged, and smoking cessation should be encouraged.
2. GI
2.1. increased risk of aspiration
2.1.1. the lower esophageal and pyloric sphincters lose muscle tone as a person ages which can cause incomplete closing and opening of the sphincters. This can cause not all the digested food to empty the stomach, and cause food in the stomach to enter back into the esophagus
2.1.2. esophageal motility decreases with age due to the smooth muscle weakening. this causes problems with swallowing food properly
2.1.3. the epiglottis, which covers the opening to the lungs may not close all the way in older age, which can lead to food and fluids entering into the lungs
2.1.4. older adults are also more likely to loose their teeth which can be aspirated or swallowed
2.1.5. older adults may also have difficulty chewing related to tooth loss or a disease process, which can lead to aspiration
2.1.6. nursing considerations- a swallow study may be necessary if there are concerns of aspiration. thickened liquids can be used to help prevent aspiration. teach the patient to sit up right and thoroughly chew food before swallowing
2.2. increased risk of indigestion
2.2.1. older adults often have decreased gastric emptying time and slower GI motility which can lead to indigestion
2.2.2. the stomach mucosa and lining thin with age, which can make the stomach sensitive to certain foods and spices
2.2.3. nursing considerations- eat small frequent meals, avoid irritating foods, sit up right when eating and don't eat less than 2 hours before going to sleep. antacids can be helpful to those with high acid content or irritation from acid
2.3. increased risk of constipation
2.3.1. gastric motility decreases therefore constipation may occur
2.3.2. dehydration and medications may cause constipation
2.3.3. the smooth muscles around the GI tract and the sphincters may lose tone and this can cause the inability to pass stools
2.3.4. nursing considerations- drink fluids, ambulate, stool softeners or laxatives may be prescribed. Certain foods may cause constipation, but every patient is different.
3. Musculoskeletal
3.1. shortened vertebrae
3.1.1. in between the vertebrae are intervertebral disks which acts as a gel-like cushion between each vertebrae
3.1.2. overtime the fluid in these disks decrease and causes the vertebrae to be aligned closer together, which can even cause grinding and deterioration of the vertebrae if the disks become small enough.
3.1.3. this causes the spine to shorten gradually over time, causing a shorter stature
3.1.4. nursing considerations- inform clients that it is normal to decrease in height as you age due to the lack of fluid in these disks. Also inform the patient that if the disks are worn down it may cause pain and discomfort that may require an analgesic.
3.2. decreased in muscle strength
3.2.1. the strength of muscles decreases over time because the muscle and muscle fibers begin to atrophy
3.2.2. the amount of lean body mass also decreases in older adults and replaced with tough fibrous tissue, fat, and lipofuscin
3.2.3. nursing considerations- tell patient it is normal not to be as strong as they were when they were younger but they should still exercise daily to help prevent and slow muscle atrophy, and overall improve body health
3.3. increase in risk for fractures
3.3.1. the bone mass and density in older adults is less than that of a younger adult which makes them easier to fracture or break
3.3.2. calcium, phosphorus, and other mineral deposits decreases in older adults making their bones less dense and strong. this can cause brittle bones.
3.3.3. nursing considerations- homes should be evaluated for falling hazards. Gait should also be assessed and the patient should be taught interventions to promote safety
4. Nervous
4.1. decrease in weight of brain
4.1.1. the weight of the brain gradually and slightly decreases with age
4.1.2. the decrease in the amount of neurons, never fibers, and nervous tissue decreases, leading to the a decrease in weight
4.1.3. over time the brain begins to atrophy and becomes smaller
4.1.4. nursing considerations- the decrease in size and weight of the brain doesn't mean neurological impairments such as demntia will occur
4.2. slower nerve responses
4.2.1. the amount of neurons an nerves present throughout the body and within the brain decrease, causing a smaller amount of available nerves to transmit messages to
4.2.2. the nerves can breakdown and be damaged over time which can cause a longer delay in responses
4.2.3. the messages have to travel back and forth from the body and brain to have a neurological response and these messages and impulses take longer to travel causing slower responses
4.2.4. nursing considerations- when assessing reflexes they may be slightly delayed or a little weaker, but they should still be present. It is important to teach about safety especially with movement.
4.3. higher risk of plaques and tangles forming on the brain
4.3.1. as nerves breakdown with age, waste products are formed
4.3.2. lipofuscin is a brown fatty pigment that may also build up in the brain
4.3.3. the presence of nerve waste products and lipofuscin can form plaques and tangles which may or may not affect memory and cognition
5. Endocrine
5.1. thyroid gland activity decreases
5.1.1. the thyroid gland is located in he neck and it produces hormones that control metabolism
5.1.2. the metabolism decreases from the decrease in amount of hormones secreted by the thyroid gland
5.1.3. in older adults the thyroid gland may also become nodular (lumpy)
5.1.4. thyroid function tests still may appear normal even with a decrease in thyroid gland's secretion. Thyroid gland hormones are typically excreted and metabolized at the same rate; therefore, the lab may still appear to be in the normal range
5.1.5. nursing considerations- a decrease in metabolism may decrease the amount of food the body needs to consume. However the about the same amount of nutrients and vitamins are needed.
5.2. a decrease in aldosterone can cause fluid and electrolyte imbalance such as a decrease in fluid, sodium, and potassium in the body. Low levels of aldosterone can cause these to be excreted instead of maintained in the body.
5.3. aldosterone and cortisol secretion decreases
5.3.1. aldosterone and cortisol are released from the adrenal glands, which are located on top of the kidneys
5.3.2. aldosterone regulates fluid and electrolyte balance and cortisol is the "stress response" hormone that breaks down glucose, fat, and protein. Cortisol also has anti-inflammatory and anti-allergy effects
5.3.3. a decrease in cortisol can inhibit the release of glucose for energy in a stressful situation. cortisol breaks down glucose, fat, and protein stores in order to provide the body with energy. the amount or cortisol in the blood remains the same but less is excreted.
5.3.4. nursing considerations- signs and symptoms of low aldosterone levels include:lightheadedness, dehydration, hypotension, and orthostatic hypotension.
5.4. ability to metabolize glucose decreases
5.4.1. insulin release by Beta cells is delayed and insufficient
5.4.2. decreases in the amount of insulin secreted causes higher glucose levels since less glucose is being broken down
5.4.3. since insulin release can be delayed there might be a spike in blood glucose and it might take longer for the body to return to a norml level
5.4.4. nursing considerations- some people who don't have a history of diabetes may need insulin in old age due to the glucose not being broken down efficiently. patients who were diabetics might have worsening of diabetes as the age and adjustments to insulin therapy may be necessary.
6. Integumentary
6.1. skin elasticity decreases
6.1.1. the process of decreasing elasticity of skin is called elasticosis
6.1.2. parts of the skin that have had sun exposure typically have less elastin
6.1.3. the decrease in elastin and connective tissue changes can make the skin become less stretchy and have a leathery texture or appearance
6.1.4. nursing considerations- if a patient needs a skin graft after a procedure it would be harder to autograft and a bigger area may need to be taken out since the skin wont stretch much during grafting. Sun exposure should be reduced by wearing sunscreen.
6.2. amount of subcutaneous fat decreases
6.2.1. over time the amount of subcutaneous fat under the skin decreases and the fat thins or is broken down.
6.2.2. the decrease in this fat causes less heat insolation and padding
6.2.3. nursing considerations- remind the patient that they are more likely to have trouble regulating body temperature and keeping heat in. Inform the patient that they are at a higher risk for injury since there is less cushion protecting underlying bones, muscles, and organs.
6.3. skin appearance may change to a paler and more translucent color
6.3.1. the amount of melanocytes in skin decrease with age. These melanocytes are responsible for coloration and a decrease can cause a more pale appearance
6.3.2. the remaining melanocytes may increase in size, which can cause age spots or other pigmented spots on the skin. These are most commonly found in sun exposed areas.
6.3.3. the epithelial cells of the skin decrease and causes the skin to thin. That along with the decrease in subcutaneous fat can cause a thin and translucent appearance.
6.3.4. nursing considerations- inform patients that age spots may occur but will most likely be on the arms legs and face. Notify them that it is normal for a gradual change of paler skin to occur. Remind them that since their skin is thinner, bruising and bleeding may occur more easily.
6.4. decrease in oil produced by sebaceous glands
6.4.1. the amount of oil produced decreases in both men and women but decreases a greater amount in women.
6.4.2. after menopause the amount of oil these glands produce start to decline due to hormonal changes
6.4.3. men have a slight decrease in the amount of oil that is produced and this starts at about the age of 80 for most men
6.4.4. nursing considerations- inform patients that without this oil their skin may feel dry and itchy. Staying hydrated and using lotion may help with dry itchy skin.
7. human needs changes
7.1. nutrition
7.1.1. nutrition impacts health and functional capacity
7.1.2. older adults have a reduced need for calories due to lean body mass, lower activity level, and lower basal metabolic rate
7.1.3. nutritional supplements may be used to treat deficiencies from disease, diet, or medications
7.1.4. adequate hydration is very important in older adults and they make consume less fluids because their thirst reflex is diminished
7.1.5. nursing considerations- offer water frequently, keep track of intake and output, and keep a food diary if nutritional deficiencies are suspected
7.2. sleep
7.2.1. lack of sleep is associated with risks of physical and mental health
7.2.2. sleep is important and affects health and well-being
7.2.3. older adults have more time in stage 1 and 2 and less time in 3 and 4
7.2.4. sleep disorders may cause insomnia, leg movements, and sleep apnea
7.2.5. certain medications and medical conditions may cause sleep disturbances. These include GERD, dementia, depression, diabetes, diuretics, beta-blockers, steroids, caffeine, and alcohol
7.2.6. nursing considerations- keep a sleep journal if any sleeping abnormalities are present, teach the patient to avoid alcohol or caffeine especially before bed, and avoid late dinners.
7.3. sexuality
7.3.1. older adults can and do enjoy sex
7.3.2. sexuality must be viewed in the context of individuals' total life experience
7.3.3. sexuality encompasses physical acts as well as caring, love, warmth, and exchange of words and touch
7.3.4. most older adults can be sexuality active but they may face barriers such as: unavailability of a partner, negative attitudes from society, concerns about body image, and medical conditions
7.3.5. nursing considerations- inform patients that they may face barriers with sexuality but most older adults are capable of a sex life.
7.4. spirituality
7.4.1. transcends and connects us to a higher power and other living organisms
7.4.2. spiritual needs include: love, meaning/purpose, hope, dignity, forgiveness, gratitude, transcendence, and expression of faith
7.4.3. strong spiritual beliefs can facilitate health and healing
7.4.4. nurses should facilitate hope and promote a patient's spirituality
7.4.5. nursing considerations- inform your patients that spirituality is important and that spirituality isn't always based on relgion.
8. Respiratory
8.1. calcification of coastal cartilage and trachea
8.1.1. hyaline cartilage forms these structures
8.1.2. 60-78% of this cartilage's weight is from water since it is a highly hydrated cartilage
8.1.3. during aging the matrix of the cartilage is dehydrated, which leads to a more fibrocartilage matrix
8.1.4. dehydrated cartilage can lead to calcification
8.1.5. nursing considerations- chest expansion may decrease because the ribs are more rigid and stiff. Rib pain may occur due to calcification.
8.2. reduction of cough and laryngeal reflexes
8.2.1. laryngeal reflex-the reflex is coughing from irritation of the larynx or fauces
8.2.2. cough reflex- the reflex to cough when there is irritation, blockage, or increase in mucus in the airway
8.2.3. these reflexes are used to detect an irritant and then expel it from the respiratory system
8.2.4. the main reason this reflex is reduced in older adults is because their sensitivity to substances that would promote the cough reflex isn't detected as easily
8.2.5. the muscles that produce the cough may also atrophy or weaken in old age which can reduce the force of the cough.
8.2.6. nursing considerations- a decreased laryngeal and cough reflexes increases the risk for aspiration so aspiration precautions may be necessary. They are also more susceptible to a bronchopulmonary infection due to not coughing out the bacteria before it multiplies and causes an infection.
8.3. increased residual capacity and decreased vital capacity
8.3.1. vital capacity is the greatest volume of air that can be expelled from the lungs after taking the deepest possible breath
8.3.2. vital capacity decreases in older adults because the lungs become less elastic, which leads to the lungs not being able to inhale and exhale as much air as the average younger adult. Also vital capacity is partially dependent on the strength of the diaphragm, which decreases in strength with aging. The diaphragm won't push up on the lungs enough to force more air out.
8.3.3. residual capacity is is the volume of air present in the lungs at the end of passive expiration
8.3.4. residual capacity increases for the same reason vital capacity decreases. The lung elasticity increases the amount of air still present in the lungs after exhale because the lungs don't compress as much. Also the diaphragm weakens and doesn't push as much air out.
8.3.5. nursing considerations- gas exchange may be altered and spO2 levels should be monitored. Smoking can worsen these values and cessation should be encouraged.
8.4. high risk of respiratory infection
8.4.1. many of the above factors increases the risk of infection.
9. Urinary
9.1. GFR decreases
9.1.1. GFR is the glomerular filtration rate, which measures how well and quickly the kidneys are filtering blood
9.1.2. blood is transported to the kidneys through the hepatic artery to be filtered by the kidney
9.1.3. nephrons are the functional units of the kidney that are responsible for filtering the blood. the number of nephrons present decreases with old age, which decreases the GFR
9.1.4. during filtration wast is removed from the blood and turned into urine and excreted. the rest of the blood is returned to the blood stream
9.1.5. nursing considerations- drugs will take longer to be excreted from the body so half-lives of medications may be increased and the risk for medication toxicity may occur.
9.2. bladder capacity decreases
9.2.1. overtime the tissues that form the bladder wall stiffens and become less elastic
9.2.2. if the bladder walls are less elastic the bladder can't stretch as much to hold the urine so the bladder capacity decreases
9.2.3. nursing considerations- fluids should be spaced out more instead of large boluses, every 2 hours the nurse should offer to take the patient to the bathroom
9.3. increase in frequency and urgency
9.3.1. the decreased bladder capacity increases the frequency because if you can't hold as much urine and still produce the same amount the frequency increases
9.3.2. the sensation of the urge to urinate decreases with age; therefore, many older adults don't feel the urge to urinate until a few minutes before they no longer can hold the urine
9.3.3. the detrusor muscle of the bladder weakens with age, which causes urgency to increase because the muscle can't contract as strong or for as long to keep the urine in the bladder
9.3.4. nursing considerations- the number one cause of falls is from getting up to use the bathroom, increases in frequency and urgency increases fall risk, offer to help the patient ambulate to the restroom every 2 hours, and be aware of possible incontinence if the patient is on diuretics
10. Immune
10.1. cell-mediated immunity decreases
10.1.1. in older adults, the time it takes to have a cell-medicated immune response
10.1.2. it takes longer for the body to sense the need for an immune response and actually respond fully
10.1.3. nursing considerations- the patient may take longer to get rid of the causative organism which can delay recovery, longer treatment may be required
10.2. risk for infection increases
10.2.1. since a lot of older adults have a weaker immune system they can't fight off infections as efficiently
10.2.2. a longer immune response time can lead to the immune system not protecting against the infection until the infection is already active within the body
10.2.3. over time the amount of immune cells decreases, which decreases the ability for the body to fight off infection
10.2.4. nursing considerations- inform the patient of the importance of hand washing, tell older adults to limit exposure to infectious agents as much as possible, and report any signs of infection as soon as possible
10.3. inflammatory defenses decrease and inflammation presents atypically
10.3.1. over time the amount of inflammatory cells decreases, which therefore decreases the effectiveness of inflammatory defenses
10.3.2. the decline in T-cell function due to age related defects is the main factor that decreases inflammatory defenses
10.3.3. nutrition can affect the immune and inflammatory response. Without proper nutrition and adequate amounts essential nutrients, the immune system may decline
10.3.4. fever may not be present in older adults with inflammation
10.3.5. some symptoms of inflammation and infection include nonspecific and vague declines in function or mental status, decreased appetite, incontinence, falls, fatigue,and exacerbation of chronic illness
10.3.6. nursing considerations- report all symptoms to a health care giver since inflammation and infection may not present with the same symptoms that occurred earlier in life. Just because a fever is not present does not mean that inflammation or infection is not present. It may take longer and more aggressive treatment for infections in older adults.
11. Reproductive
11.1. Male
11.1.1. seminal vesicles develop thinner epithelium
11.1.1.1. teach the patient that the seminal vesicles are responsible for the fluid that mixes with sperm,
11.1.1.2. over time and after use the tall columnar epithelium of the seminal vesicles start to thin
11.1.1.3. the seminal vesicles' epithelium and mucosal folds also startto shrink
11.1.1.4. nursing considerations- less fluid may be excreted through these tubes but that is a normal finding and it typically doesn't effect the ability to engage in sexual intercourse
11.1.2. enlargement of the prostate
11.1.2.1. the prostate is the gland that produces the fluid that carries the sperm during ejaculation
11.1.2.2. benign prostatic hyperplasia (BPH) involves the enlargement of the prostate which can obstruct urine flow as the prostate increases in size
11.1.2.3. nursing considerations- tell patients to report symptoms of BPH which include: inability to urinate, dribbling at the end of urination, incomplete emptying of the bladder, straining to urinate, and weak urine stream
11.1.3. ejaculation fluid contains less live sperm
11.1.3.1. over time the amount of sperm the testicles produces decreases, which leads to less sperm being in ejaculation fluid
11.1.3.2. nursing considerations- in older age fertility decreases because of the decrease in the amount of sperm
11.2. Female
11.2.1. vulva atrophies
11.2.1.1. when women pass menopause and into older age the amount of estrogen in the body decreases
11.2.1.2. a decrease in estrogen can cause thinning, drying, and inflammation of the vulva
11.2.1.3. nursing considerations- this is a normal finding as women age, but can cause discomfort during intercourse
11.2.2. vaginal epithelium thins
11.2.2.1. over time the epithelium in the vagina begins to thin due to a decrease in estrogen levels
11.2.2.2. nursing considerations- the thinner epithelium may cause discomfort during intercourse and drying may also occur
11.2.3. uterus and ovaries decrease in size
11.2.3.1. after menopause the ovaries don't need to secrete as much hormones and shrink about 3 cm
11.2.3.2. after menopause the amount of estrogen in the body drastically decreases and the uterus is no longer needed to hold a fetus. The tissues and muscles thin and shrink
11.2.3.3. nursing considerations- after menopause women can no longer become pregnant and menses will stop . the shrinking of these organs doesn't effect the ability to engage in intercourse

