1. Due to Two types:
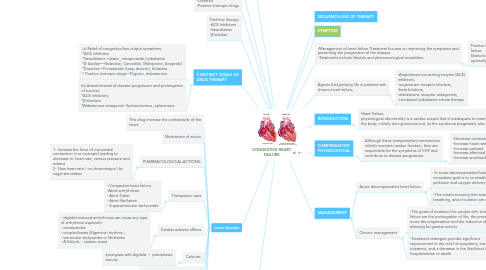
1.1. 2) Diastolic dysfunction - increased ventricular stiffness, ventricular hypertrophy, infiltrative myocardial disease, myocardial ischemia and MI, mitral or tricuspid valve stenosis and pericardial disease -results in ventricle does not fill adequately and decrease cardiac out put (Increased workload imposed on heart)
1.2. Compensatory mechanisms: 1)Tachycardia and increased contractility through sympathetic nervous system activation. 2)The Frank-Starling mechanism, whereby increased preload increases stroke volume 3)Vasoconstriction (due to Activation of renin-angiotensin system) 4)Ventricular hypertrophy and remodeling.
1.2.1. Symptoms -Tachycardia(abnormally rapid heart rate) -Decrease exercise tolerance -Cardiomegaly (abnormal enlargement of the heart) -Dyspnea/Shortness of breath -Fatigue -Fluid retention/congestion Pulmonary edema Peripheral edema
1.3. Verapamil, diltiazem, captopril, propafenone and amiodarone
1.3.1. increase plasma concentration of digoxin → plasma concentration of digoxin is doubled → toxicity can occur.
1.4. 1)Systolic dysfunction -reduction in muscle mass, dilated cardiomyopathies, and ventricular hypertrophy. -results in ventricle unable to pump blood effectively.
2. cause hypokalemia which increases the risk of digitalis arrhythmias; potassium supplements should be given prophylactically.
3. Second-line therapy -Diuretics -Positive Inotropic drugs
4. First-line therapy -ACE inhibitors -Vasodilators -β blocker
5. 2 DISTINCT GOALS OF DRUG THERAPY
5.1. (a) Relief of congestive/low output symptoms: *ACE inhibitors *Vasodilators -nitrate,, nitroprusside,hydralazine *β blocker—Nebivolol, Carvedilol, Metoprolol, bisoprolol *Diuretics—Furosemide (Loop diuretic), thiazides * Positive Inotropic drugs—Digoxin, dobutamine
5.2. (b) Arrest/reversal of disease progression and prolongation of survival: *ACE inhibitors, *β blockers *Aldosterone antagonist- Spironolactone, eplerenone
6. SEQUENCE-LINE OF THERAPY
7. Cardiac Glycosides
7.1. This drug increase the contractality of the heart.
7.2. Mechanism of action
7.3. PHARMACOLOGICAL ACTIONS:
7.3.1. 1- Increase the force of myocardial contraction (+ve inotropic) leading to decrease in: heart size, venous pressure and edema 2- Slow heart rate ( -ve chronotropic ) by vagal stimulation
7.4. Therapeutic uses
7.4.1. - Congestive heart failure -Atrial arrhythmias: - Atrial flutter - Atrial fibrillation - Supraventricular tachycardia
7.5. Cardiac adverse effects
7.5.1. - digitalis-induced arrhythmias can cause any type of arrhythmia especially: - extrasystoles - coupled beats (Bigeminal rhythms ) - ventricular tachycardia or fibrillation - A.V.block, - cardiac arrest.
7.6. Calcium:
7.6.1. synergises with digitalis → precipitates toxicity.
7.7. Inhibit Na + / K + ATPase enzyme
7.8. Extra cardiac adverse effects
7.8.1. -GIT : common ( the earliest signs of toxicity ): Anorexia,nausea, vomiting, diarrhea CNS: Headache, visual disturbances, drowsiness
7.9. Factors that increase digitalis toxicity: - Small Lean body mass - Renal diseases - Hypothyroidism - Hypokalemia - Hypomagnesemia - Hypercalemia
8. DRUG INTERACTION
8.1. Diuretics:
8.2. Propranolol, verapamil, diltiazem and disopyramide:
8.2.1. may additively depress A-V conduction and oppose positive inotropic action.
8.3. Adrenergic drugs:
8.3.1. can induce arrhythmias (both increase ectopic automaticity).
8.3.2. can induce arrhythmias in digitalized patients.
8.3.3. absorption is increased by atropinic drugs.
8.4. Digoxin
8.4.1. Succinylcholine:
8.4.2. Q
9. SYMPTOM
10. -Management of heart failure Treatment focuses on improving the symptoms and preventing the progression of the disease. -Treatments include lifestyle and pharmacological modalities.
10.1. Positive inotropic drugs, very helpful in acute failure. Diastolic dysfunction does not usually respond optimally to positive inotropic drugs
11. Agents that prolong life in patients with chronic heart failure;
11.1. -Angiotensin-converting enzyme (ACE) inhibitors, -angiotensin receptor blockers, -beta blockers, -aldosterone receptor antagonists, -combined hydralazine-nitrate therapy
12. INTRODUCTION
12.1. Heart Failure physiological abnormality is a cardiac output that is inadequate to meet the metabolic demands of the body, initially during exercise but, as the syndrome progresses, also at rest.
13. COMPENSATORY PHYSIOLOGYCAL
13.1. Although these compensatory mechanisms initially maintain cardiac function, they are responsible for the symptoms of CHF and contribute to disease progression.
13.1.1. -Decrease contractility -Increase heart rate -Increase preload -Increase afterload -Increase workload of heart
14. MANAGEMENT
14.1. Acute decompensated heart failure
14.1.1. -In acute decompensated heart failure, the immediate goal is to re-establish adequate perfusion and oxygen delivery to end organs.
14.1.2. -This entails ensuring that airway, breathing, and circulation are adequate.
14.2. Chronic management
14.2.1. -The goals of treatment for people with chronic heart failure are the prolongation of life, the prevention of acute decompensation and the reduction of symptoms, allowing for greater activity.
14.2.2. -Treatment strategies provide significant improvement in the relief of symptoms, exercise tolerance, and a decrease in the likelihood of hospitalization or death.

