Pneumonia
por walid naseer
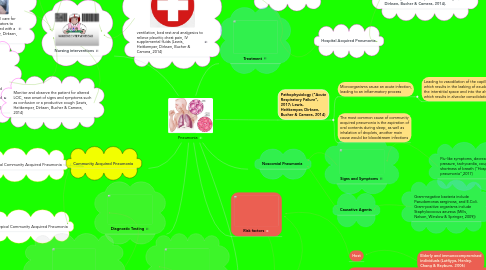
1. Signs and Symptoms
1.1. Slower and more insidious onset with a nonproductive cough, mild fever, chest pain (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
2. Causative Agents
2.1. Chlamydophilla Pneumoniae, influenzavirus, RSV, Chlamydia, Mycoplasma pneumonia (Thibodeau & Viera, 2004)
3. Signs and Symptoms
3.1. Pleuritic Chest pain, Rapid onset of fever, productive cough, tachycardia, crackles upon ausculation, fluid build up increasing tactile fremitus( Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
4. Causative Agents
4.1. Bacterial agents such as streptococcus (Lutfiyya, Henley, Chang & Reyburn, 2006)
5. Typical Community Acquired Pneumonia
6. Atypical Community Acquired Pneumonia
7. Encourage adequate rest with moderate activity. Promote adequate nutritional intake (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
8. Institute isolation precautions as appropriate (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
9. Review with patients the importance of the cessation of smoking, alcohol and substance abuse (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
10. ventilation, bed rest and analgesics to relieve pleuritic chest pain, IV supplemental fluids (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
11. It is important to provide oral care for patients on respiratory ventilators to prevent pneumonia associated with a ventilator (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
12. Patient teachings are encouraged about effective coughing techniques, proper diet, and fluid intake (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
13. Monitor and observe the patient for altered LOC, new onset of signs and symptoms such as confusion or a productive cough (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
14. Laboratory Testing Findings
15. Chest Radiography is the number one diagnostic testing used in order to find if there is any fluid present in the lungs (Lutfiyya, Henley, Chang & Reyburn, 2006)
16. To look for any positive gram stains, an increase in WBC, and lastly if blood cultures are positive (Lutfiyya, Henley, Chang & Reyburn, 2006)
17. living conditions (Baik, Curhan, Rimm, Bendich, Willett & Fawzi, 2000)
18. Diagnostic Testing
19. Nursing interventions
20. Community Acquired Pneumonia
21. Targets bacterial pneumococcal pneumonia, H,influenzae, enteric gram-negative bacilli. The main drug choice is fluoroquinolonnes. (Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014).
22. Signs and Symptoms
23. Causative Agents
24. Flu-like symptoms, decreased blood pressure, tachycardia, cough, chest pain, shortness of breath ("Hospital-acquired pneumonia",2017)
25. Gram-negative bacteria include Pseudomonas aerginosa, and E.Coli. Gram-positive organisms include Staphylococcus aeureus (Mills, Nelson, Winslow & Springer, 2009))
26. Elderly and immunocompromised individuals (Lutfiyya, Henley, Chang & Reyburn, 2006)
27. Co-morbidities
28. Host
29. Life-style factors
30. Smoking (Baik, Curhan, Rimm, Bendich, Willett & Fawzi, 2000)
31. Alcohol or substance abuse (Baik, Curhan, Rimm, Bendich, Willett & Fawzi, 2000)
32. Respiratory issues such as Asthma, COPD, Cystic fibrosis, Diabetes, and heart disease. (Farr, Bartlett, Wadsworth & Miller, 2000)
33. The treatment involves adminstering an anti-pneumococcal beta-lactam antibiotic, as well as macrolies such as clarithromycin (Baer, 2017)
34. Hospital Acquired Pneumonia
35. In an outpatient setting treatment involves a macrolides which reduce the chances of anti-biotic resistance (Lutfiyya, Henley, Chang & Reyburn, 2006)
36. Community Acquired Pneumonia
37. Noscomial Pneumonia
38. Treatment
39. Pathophysiology ("Acute Respiratory Failure", 2017; Lewis, Heitkemper, Dirksen, Bucher & Camera, 2014)
39.1. Microorganisms cause an acute infection, leading to an inflammatory process
39.1.1. Leading to vasodilation of the capillaries which results in the leaking of exudate into the interstitial space and into the alveoli which results in alveolar consolidation
39.1.1.1. This further exacerbates into hypoxemia and hypercapnia which can be identified as a type 2 respiratory failure
39.1.1.1.1. In young patients it is seen as short of breath, painful near the chest region and a productive cough with a fever
39.1.1.1.2. In older individuals it is seen with reduced productive coughing, same quality of pain in the chest region, and reduced mental impairments such as confusion or lethargy
