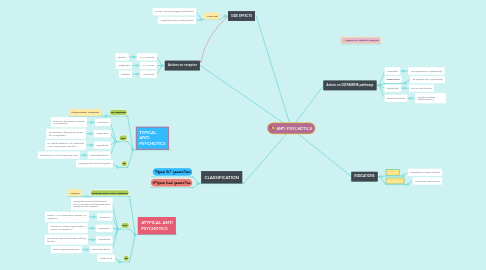
1. Actions on receptor
1.1. M1, a1 receptor
1.1.1. Sedation
1.2. H1 + 5HT2C
1.2.1. Weight gain
1.3. M3 receptor
1.3.1. Diabetes
2. CLASSIFICATION
2.1. Typical (1st generation)
2.2. Atypical (2nd generation
3. SIDE EFFECTS
3.1. Acute onset
3.1.1. On EPS, causing iatrogenic parkinsonism
3.1.2. Cognitive toxicity, causing delirium
4. TYPICAL ANTI PSYCHOTICS
4.1. D2 Antagonist
4.1.1. Chlorpromazine, Haloperidol
4.2. MOA
4.2.1. Mesolimbic
4.2.1.1. blocks DA transmission, improve +ve symptoms
4.2.2. Mesocortical
4.2.2.1. D/t existing DA hypoactivity, worsen the -ve symptoms
4.2.3. Nigrostriatal
4.2.3.1. DA inhibits release of ACh, bloackade of DA may increase risk of EPS
4.2.4. Tuberoinfundibular
4.2.4.1. Blockade of DA, will increase PRL level
4.3. SE
4.3.1. Extrapyramidal SE (*neurological)
5. ATYPICAL ANTI PSYCHOTICS
5.1. Serotonin (5HT2) 2A/D2 Antagonist
5.1.1. Clozapine
5.2. MOA
5.2.1. Has greater functional blockade for 5HT2A receptors, and dissociate more rapidly from D2 receptors
5.2.2. Mesolimbic
5.2.2.1. Blocks >> DA transmission, improve +ve symptoms
5.2.3. Mesocortical
5.2.3.1. Increase DA release, high enough to improve -ve symptoms
5.2.4. Nigrostriatal
5.2.4.1. Reverses enough D2 blockade, reducing the EPS
5.2.5. Tuberoinfundibular
5.2.5.1. Reduce hyperprolactinemia
5.3. SE
5.3.1. Metabolic SE
6. Action on DOPAMINE pathways
6.1. Mesolimbic
6.1.1. +ve symptoms (DA hyperactivity)
6.2. Mesocortical
6.2.1. -ve symptoms (DA hypoactivity)
6.3. Nigrostriatal
6.3.1. EPS & motor function
6.4. Tuberoinfundibular
6.4.1. Prolactin secretion (inhibited by DA)
7. Keyword: DA stands for dopamine
8. INDICATIONS
8.1. Psychiatric
8.1.1. Schizophrenia, bipolar disorder
8.2. Non psychiatric
8.2.1. Anti-emetic, relief pruritus

