1. OPIODS
1.1. highly potent, very effective, reliable, work rapidly, available PO/IM/IV/transdermal/Nasal
1.2. SIDE EFFECTS:
1.2.1. RESPIRTAORY DEPRESSION
1.2.2. N/V
1.2.3. CONSTIPATION
1.2.3.1. all patients on narcotics need a bowel regimen
1.2.3.2. docusate 100 mg BID + senna 2 tabs qHs
1.2.3.3. lactulose 30 ml qd
1.2.3.4. polyethylene glycol 2 tbs qd
1.2.4. PRURITUS
1.2.5. MENTAL STATUS CHANGE
1.2.6. URINARY RETENTION
1.2.7. ORTHOSTATIC HYPOTENSION
1.2.8. DEPENDENCE
1.2.8.1. when you stop the drug you have withdrawl symptoms
1.2.9. TOLERANCE
1.2.9.1. increased amounts of drug are required to produce the same efficacy
1.2.10. ADDICTION
1.2.10.1. chronic disease with lack of control over drug use
1.2.10.2. psuedoaddiction - iatrogenic syndrome due to misinterpretation of pain relief seeking behavior with drug seeking behavoir
1.2.11. ABUSE
1.2.11.1. use of medication deviated from medical & legal standards
1.3. FIRST LINE
1.3.1. MORPHINE (Avinza, DepoDur, Duramorph, Astramorph, Kadian)
1.3.1.1. immediate and controlled release
1.3.1.2. morphine mg equivalents
1.3.1.2.1. 30 mg PO or 10 mg IV
1.3.2. OXYCODONE
1.3.2.1. Oxycontin - long acting
1.3.2.1.1. PERCOCET - oxycodone & acetaminophen
1.3.2.1.2. PERCODAN - oxycodone & aspirin
1.3.2.2. immediate and controlled released
1.3.2.3. TREATMENT INDICATIONS AND GOALS
1.3.2.4. STARTING DOSE
1.3.2.4.1. 1.5 MME
1.3.3. HYDROCODONE
1.3.3.1. Vicodin, Lortab
1.3.3.1.1. VICODIN - hydrocodone and acetameinophen 5/500
1.3.4. FENTANYL
1.3.4.1. Duragesic, Sublamaze
1.3.4.2. patch
1.3.4.2.1. 25 mcg/hr
1.3.4.3. 2.4 MME
1.4. SECOND LINE
1.4.1. HYDROMORPHONE
1.4.1.1. Dilaudid
1.4.1.2. STARTING DOSE
1.4.1.2.1. 1 MME
1.4.2. METHADONE
1.4.2.1. Dolophine
1.5. THIRD LINE
1.5.1. MEPERIDINE
1.5.1.1. Demerol
1.5.1.2. toxic metabolite - cannot keep escalating doses
1.5.2. CODEINE
1.5.2.1. Tylenol with Codeine
1.5.2.2. STARTING DOSE
1.5.2.2.1. .15 MME
2. OPIOD ANTAGONISTS
2.1. FIRST LINE
2.1.1. NALOXONE
2.1.1.1. Narcan
2.2. SECOND LINE
2.2.1. METHYLNALTREXONE
2.2.1.1. Relistar
2.2.1.2. Peripheral μ opiod receptor antagonist
2.2.1.3. REFRACTORY CONSTIPATION FROM NARCOTSC
2.2.1.4. SQ
2.2.2. NALTREXONE
2.2.2.1. ReVia
3. ANALGESICS
3.1. FIRST LINE
3.1.1. TRAMADOL
3.1.1.1. Ultram
3.1.1.2. synthetic codeine analogue
3.1.1.2.1. mu opioid receptor agonist
3.1.1.2.2. NE and SR reuptake inhibitor
3.2. SECOND LINE
3.2.1. TAPENTADOL
3.2.1.1. Nucyntal
3.2.1.2. Mu agonist and NE reuptake inhibitor
3.2.2. ZINCONOTIDE
3.2.2.1. Prialt
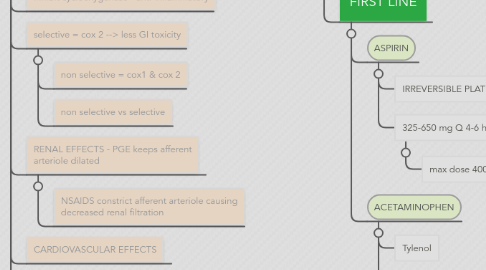
4. NSAIDS
4.1. inhibit cyclooxygenase - anti-inflammatory
4.2. selective = cox 2 --> less GI toxicity
4.2.1. non selective = cox1 & cox 2
4.2.2. non selective vs selective
4.3. RENAL EFFECTS - PGE keeps afferent arteriole dilated
4.3.1. NSAIDS constrict afferent arteriole causing decreased renal filtration
4.4. CARDIOVASCULAR EFFECTS
4.5. FIRST LINE
4.5.1. IBUPROFEN
4.5.1.1. Advil, Motrin
4.5.1.2. 325 - 650 mg Q 4-6 hrs
4.5.1.2.1. max dose - 32000 mg acute, 2400 chronic
4.5.2. NAPROXEN
4.5.2.1. Aleve
4.5.2.2. SAFEST IN PATIENTS WITH CARDIAC DISEASE
4.5.2.3. 250 mg Q 8 hours
4.5.2.3.1. 1250 mg acute, 1000 chronic
4.5.3. MELOXICAM
4.5.3.1. Mobic
4.5.3.2. GIVEN ONCE A DAY
4.5.3.3. 7.5 - 15 mg QD
4.5.3.3.1. max dose 15 mg
4.6. SECOND LINE
4.6.1. CELECOXIB
4.6.1.1. Celebrex
4.6.1.2. COX2 SELECTIVE
4.6.1.3. BLACK BOX WARNING FOR HEART ATTACK
4.6.1.3.1. BLOCK VASODILATION EFFECT IN ARTERIOLES
4.6.1.4. 200 mg QD or 100 mg Q 12 hrs
4.6.1.4.1. 400 mg (increased CV risk > 200 mg)
4.6.1.5. CONTRAINDICATED FOR TREATMENT OF PERI-OPERATIVE PAIN FROM CABG
4.6.2. INDOMETHACIN
4.6.2.1. Indocin
4.6.2.2. GOUT
4.6.2.3. 25 mg Q 8-12 hrs OR 75 mg 1-2x daily
4.6.2.3.1. max dose 150 mg
4.6.3. KETORALAC
4.6.3.1. Toradol
4.6.3.2. CAN BE GIVEN IV OR IM
4.6.3.3. 15-30 mg Q 6 hrs
4.6.3.3.1. < 65 y/o 60 mg x 1
4.6.3.3.2. > 65 y/o 30 mg x 1
4.7. THIRD LINE
4.7.1. ETODOLAC
4.7.1.1. Lodine
4.7.2. KETOPROFAN
4.7.2.1. Orudis
4.7.3. MECLOFENAMATE
4.7.3.1. Meclomen
4.7.4. PIROXICAM
4.7.4.1. Feldene
5. OTHER OTC
5.1. FIRST LINE
5.1.1. ASPIRIN
5.1.1.1. IRREVERSIBLE PLATELET AGGREGATION
5.1.1.2. 325-650 mg Q 4-6 hrs
5.1.1.2.1. max dose 4000 mg
5.1.2. ACETAMINOPHEN
5.1.2.1. Tylenol
5.1.2.2. COX2 inhibition in CNS, block pain impulse + antipyretic effects
5.1.2.3. 325 - 1000 mg q 4-6 hours
5.1.2.3.1. max dose - 4000 mg
6. TOPICAL ANESTHETICS
6.1. FIRST LINE
6.1.1. LIDOCAINE
6.1.1.1. Xylocaine
6.1.1.2. LOCALIZED NEUROPATHIC PAIN
6.1.1.2.1. postherpetic neuralgia
6.1.1.2.2. allodynia
6.1.1.3. Used as adjunct with other meds
6.1.1.3.1. 5% LIDOCAINE PATCH
6.1.1.3.2. 5% LIDOCAINE GEL
6.2. SECOND LINE
6.2.1. BENZOCAINE
7. NEUROPATHIC PAIN
7.1. FIRST LINE
7.1.1. GABAPENTIN
7.1.1.1. Neurontin
7.1.1.2. DIZZINESS AND SEDATION
7.1.1.3. POSTHERPETIC NEURALGIA & PAINFUL DIABETIC NEUROPATHY
7.1.1.4. STARTING DOSE
7.1.1.4.1. TAKES 2 MONTHS
7.1.2. CARBAMAZEPINE
7.1.2.1. 1st line for trigeminal neuralgia
7.2. SECOND LINE
7.2.1. PREGABALIN
7.2.1.1. Lyrica
7.2.1.2. DIZZINESS & SEDATION
7.2.1.3. POSTHERPETIC NEURALGIA, PAINFUL DIABETIC NEUROPATHY, CENTRAL NEUROPATHIC PAIN, FIBROMYALGIA
7.2.1.4. STARTING DOSE
7.2.1.4.1. QUICKER ONSET HTAN GABAPENTIN
7.2.2. MILNACIPRAN
7.2.2.1. Savella
8. MUSCLE RELAXANTS
8.1. FIRST LINE
8.1.1. CYCLOBENZAPRINE
8.1.1.1. Flexeril
8.1.1.2. MOA by sedation rather than relaxation
8.1.1.3. CNS DEPRESSION
8.1.1.4. 10 mg TID
8.1.1.4.1. max dose 10-40 mg/day
8.2. SECOND LINE
8.2.1. BACLOFEN
8.2.1.1. Lioresal, Liofen, Gablofen
8.2.1.2. MOA by sedation rather than relaxation
8.2.1.3. CNS DEPRESSION
8.2.1.4. 5 mg Q day
8.2.1.4.1. titrated gradually to 5-10 mg TID
8.2.2. METHOCARBAMOL
8.2.2.1. Robaxin
8.2.2.2. MOA by sedation rather than relaxation
8.2.2.3. CNS DEPRESSION
8.2.2.4. 1500 mg 4 x daily
8.2.2.4.1. DOSE NOTES
