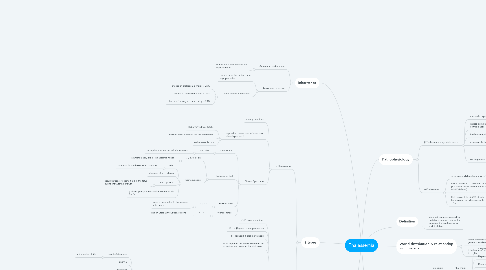
1. Inheritance
1.1. Autosomal codominant
1.1.1. carriers have thal trait and are asymptomatic
1.2. Autosomal recessive
1.2.1. carriers have the trait and are asymptomatic
1.2.2. if both parents are carriers:
1.2.2.1. chance of thalassemia major is 25%
1.2.2.2. chance of thalassemia trait is 50%
1.2.2.3. chance of having a normal baby is 25%
2. 2 types
2.1. α-Thalassemia
2.1.1. mostly deletions
2.1.2. dependent on number of deletions, phenotypes are 3
2.1.2.1. HbBart's/hydrops fetalis
2.1.2.2. HbH disease: behaves like thal intermedia
2.1.2.3. α-thalassemia trait
2.1.3. Clinical Syndrome
2.1.3.1. silent carrier
2.1.3.1.1. -/α, α/α
2.1.3.2. α-Thalassemia trait
2.1.3.2.1. -/-, α/α (asian)
2.1.3.2.2. homozygoous
2.1.3.3. HbH disease
2.1.3.3.1. -/-, -/α
2.1.3.4. Hydrops fetalis
2.1.3.4.1. -/-, -/-
2.2. β-Thalassemia
2.2.1. >200 point mutations
2.2.2. β0: no β-globin chain production
2.2.3. β+: reduced β-globin synthesis
2.2.4. each region in the world: common 5-6 mutations that account for >90 cases
2.2.5. Clinical Syndrome
2.2.5.1. major
2.2.5.1.1. homozygous
2.2.5.2. intermedia
2.2.5.2.1. variable
2.2.5.3. minor
2.2.5.3.1. heterozygous
2.2.6. Mainly point mutations that lead to defects in transcription, splicing, or translation of β-globin mRNA
3. Discriminant functions to differentiate IDA from BTT
3.1. Mentzer index: MCV/RBC
3.1.1. <13
3.1.1.1. BTT
3.1.2. >13
3.1.2.1. IDA
3.2. Shine and Lal index: MCV^2 X MCH
3.2.1. <1530
3.2.1.1. BTT
3.2.2. >1530
3.2.2.1. IDA
3.3. England-Frazer index: MCV -(Hb*5)-RBC-3.4
3.3.1. Negative value
3.3.1.1. BTT
3.3.2. Positive value
3.3.2.1. IDA
4. Definition
4.1. inherited disorders caused by mutations in globin genes that decrease the synthesis of α- and β-globin
5. World distribution & relationship with malaria
5.1. one of the most common genetic disorders
5.2. β thal carriers/heterozygous β thal
6. Pathophysiology
6.1. β-Thalassemia major/intermedia
6.1.1. microcytc hypochromic anemia
6.1.2. excess α chains get precipitated in erythroblasts
6.1.3. ineffective erythropoiesis
6.1.4. extravascular hemolysis
6.1.5. consequences
6.1.5.1. anemia
6.1.5.2. iron overload d/t increases absorption and blood transfusions
6.1.5.3. skeletal deformities - hemolytic facies
6.2. α-Thalassemia
6.2.1. α to non-α globin chain ratio is 1.0±0.05
6.2.2. lack of α-chains (--/-α) leads to an excess of β/γ chains which precipitate as tetramers (HbH/HbBart's)
6.2.3. HbH account for 5-50% of total hemoglobin in individuals with --/-α
7. Laboratory Diagnosis
7.1. Hemogram
7.1.1. thal major
7.1.1.1. 8-month old baby with failure to thrive
7.1.1.2. Hepatosplenomegaly
7.1.1.3. Reported TLC in an alternative counter
7.1.1.3.1. 44.0X10^3/100
7.1.1.4. Smear review
7.1.1.4.1. Typical thalassemia major
7.1.1.4.2. 101nRBCs/100 WBCs
7.1.1.4.3. No correction of TLC required
7.2. Peripheral smear
7.2.1. Thal trait
7.2.2. Thal major
7.3. Hb electrophoresis
7.3.1. movement of molecules under an electric charge
7.3.2. Hb at alkaline pH is negatively charged and moves from cathode to anode
7.3.3. stops at the position where charge is neutralized
7.4. HbHPLC
7.5. Family Study if the child is transfused
7.6. DNA studies: mutation analysis
7.7. Measuring HbA2
7.7.1. <3.1%
7.7.1.1. Normal
7.7.1.2. α thal trait
7.7.2. >9%
7.7.2.1. HbE syndromes
7.7.3. 3.9-9%
7.7.3.1. βTT
7.7.4. 3.1-3.9%
7.7.4.1. βTT with IDA
7.7.4.2. Interaction of α and β Thal
