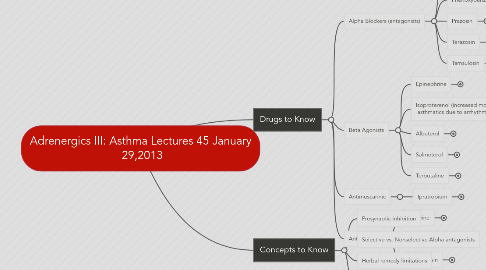
1. Drugs to Know
1.1. Alpha Blockers (antagonists)
1.1.1. Phentolamine
1.1.1.1. MOA: Competitive alpha1 and alph2 antagonists (blockers)
1.1.1.2. Clinical Use: Pheochromocytoma - controls HTN episodes; dermal necrosis; dx of pheochromocytoma.
1.1.1.3. Special Info: slow onset but lasts a long time. Binds to receptors irreversibly.
1.1.1.4. Problems: Postural hypotension, intense reflex tachycardia and the forceful contraction. Arrhythmias, ischemia, sexual dysfunction, nasal congestion.
1.1.2. Phenoxybenzamine
1.1.2.1. MOA: alpha1 and alph2 antagonists (blockers), irreversible binding!
1.1.2.2. Clinical Use: Pheochromocytoma - controls HTN episodes; dermal necrosis; dx of pheochromocytoma.
1.1.2.3. Special Info: slow onset but lasts a long time. Binds to receptors irreversibly.
1.1.2.4. Problems: Postural hypotension, intense reflex tachycardia and the forceful contraction. Arrhythmias, ischemia, sexual dysfunction, nasal congestion.
1.1.3. Prazosin
1.1.3.1. MOA: competitive alpha 1 (vs. alpha2) adrenergic antagonist. Dilates both arteries and veins. Decreases TPR
1.1.3.2. Clinical Use: HTN, and HTN w/ CHF, Benign prostatic hyperplasia (BPH); Raynaud's
1.1.3.3. Special Info: Phenobarbital shorts its half-life, the severe orthostatic hypotension patients should be lying down and observed for 2hrs after initial doses
1.1.3.4. Problems: "First dose phenomenon", Hypotension (postural) and/or syncope, sodium depletion, Edema - Must take at night before bed
1.1.4. Terazosin
1.1.4.1. Problems: "First dose phenomenon", Hypotension (postural) and/or syncope, sodium depletion, Edema - Must take at night before bed
1.1.4.2. Special Info: Phenobarbital shorts its half-life, the severe orthostatic hypotension patients should be lying down and observed for 2hrs after initial doses
1.1.4.3. Clinical Use: HTN, and HTN w/ CHF, Benign prostatic hyperplasia (BPH); Raynaud's
1.1.4.4. MOA: competitive alpha 1 (vs. alpha2) adrenergic antagonist. Dilates both arteries and veins. Decreases TPR
1.1.5. Tamsulosin
1.1.5.1. MOA: Peripheral alpha 1 adrenergic antagonist. Dilates both arteries and veins.
1.1.5.2. Clinical Use: relatively selective effect on urinary flow to treat BPH w/ lower incidence of orthostatic hypotension , and HTN w/ CHF
1.1.5.3. Special Info: Phenobarbital shorts its half-life, the severe orthostatic hypotension patients should be lying down and observed for 2hrs after initial doses
1.1.5.4. Problems: Ejaculatory dysfunction, lower amounts of Hypotension (postural), sodium depletion, Edema than prazosin or terazosin
1.2. Beta Agonists
1.2.1. Epinephrine
1.2.1.1. MOA: Adrenergic agonist causes bronchodilation (B2 receptor), vasoconstriction (a1), and decreased secretions (a1).
1.2.1.2. Clinical Use: short term/ emergency use for severe bronchoconstriction/vasodilation (anaphylaxis). Less potent than albuterol for maintenance, no prescription needed.
1.2.1.3. Problems: increased heart rate, arrhythmogenic, metabolic and GI abnormalities, CNS Stimulation
1.2.1.4. Special Info: MAO/COMT metabolizes these drugs; half-life 2mins, don't give to HTN HThyroid, cerebrovasacular insufficiency, or Narrow angle glaucoma.
1.2.2. Isoproterenol (increased mortality rate in asthmatics due to arrhythmias)
1.2.2.1. MOA: B1 and B2 agonist. Adrenergic agonist causes bronchodilation.
1.2.2.2. Clinical Use: short term/ emergency use for severe bronchoconstriction/vasodilation (anaphylaxis). Less potent than albuterol for maintenance, REQUIRE Prescription!
1.2.2.3. Problems: increased heart rate, arrhythmogenic, metabolic and GI abnormalities, CNS Stimulation
1.2.2.4. Special Info: MAO/COMT metabolizes these drugs; half-life 2mins, don't give to pts with Tachycardia. With drawl may induce reflex bronchoconstriction.
1.2.3. Albuterol
1.2.3.1. MOA: short acting (3-4hrs), Beta 2 adrenergic receptor agonist- causes bronchodilation, activates cAMP in bronchial smooth muscle.
1.2.3.2. Clinical Use: Tx acute asthma and prevent exertion asthma
1.2.3.3. Problems: cardiovascular effects: vasodilation (mild hypotension), tachycardia, tremors, CNS stimulation, inhalation preps have fewer side effects.
1.2.3.4. Special Info: Don't give with Beta blockers (heart disease pts), MAO inhibitors, TCA or other sympathomimetics. Bronchodilation severely reduced in hypoxic and acidotic pts.
1.2.4. Salmeterol
1.2.4.1. MOA: long acting, Beta 2> Beta1 adrenergic receptor agonist- causes bronchodilation, activates cAMP in bronchial smooth muscle.
1.2.4.2. Clinical Use: chronic asthma, bronchospasms in adults. NOT FOR ACUTE ATTACKS
1.2.4.3. Problems: tachycardia, mild hypotension, nasopharygitis, headache, and cough
1.2.4.4. Special Info: Don't give with Beta blockers (heart disease pts), MAO inhibitors, TCA or other sympathomimetics. Bronchodilation severely reduced in hypoxic and acidotic pts.
1.2.5. Terbutaline
1.2.5.1. MOA: short acting (3-4hrs), Beta 2 adrenergic receptor agonist- causes bronchodilation, activates cAMP in bronchial smooth muscle.
1.2.5.2. Clinical Use: Tx acute asthma and prevent exertion asthma
1.2.5.3. Problems: cardiovascular effects: vasodilation (mild hypotension), tachycardia, tremors, CNS stimulation, inhalation preps have fewer side effects.
1.2.5.4. Special Info: Don't give with Beta blockers (heart disease pts), MAO inhibitors, TCA or other sympathomimetics. Bronchodilation severely reduced in hypoxic and acidotic pts.
1.3. Antimuscarinic
1.3.1. Ipratropium
1.3.1.1. MOA: Muscarinic antagonist. Reverses acetylcholine-induced bronchoconstriction.
1.3.1.2. Clinical Use: Bonchospasm associated with COPD in adults. It is second-line therapy for Asthma. (really for patients who can't take Beta2 agonists).
1.3.1.3. Problems: Few systemic anticholinergic effects because it is a quarternery ammonium compound which cannot readily cross into the systemic circulation. -->may cause hypotension (ganglionic blockade) and muscle weakness (neuromuscular blockade)
1.3.1.4. Special Info: Don't give with narrow angle glaucoma patients, or BPH patients. It enhances the effects of adrenergic agonist.
1.4. Antitussive
1.4.1. Codeine
1.4.1.1. MOA: metabolized to morphine. agonist against mu opioid receptor, slight action at the delta and kappa (similar to morphine) codeine produces less analgesia than morphine.
1.4.1.2. Clinical Use: analgesia: mild-moterate pain especially when combined with aspirin or acetaminophen, Antitussive as well (effective in chronic cough but questions regarding acute cough). Also Antidiarrheal.
1.4.1.3. Problems: constipation; respiratory depression (rare)
1.4.1.4. Special Info: Antitussive mechanism is not well understood but appears to be mediated by diff receptors than those for analgesic effects of opioids. My be due to more of the codeine effect than morphine.
1.4.2. Dextromethorphan
1.4.2.1. MOA: D-isomer of codeine analog methorphan but NO activity at opioid receptors; NMDA receptor antagonist (blocker) but also binds elsewhere.
1.4.2.2. Clinical Use: antitussive
1.4.2.3. Problems: relatively safe at prescribed doses. High doses (>2mg/kg): tachycardia, agitation, psychosis, seizure, ataxia, coma
1.4.2.4. Special Info: FDA prohibits this drugs use in kids under 6 y/o. Patients misuse this for drug high, "Robotripping" "Robodosing", "going pharming", "Dexing". The inhibition of the NMDA receptors (ie. ketamine and PCP) causes hallucinations, and "out of body" dissociation.
1.4.3. Guaifenesin
1.4.3.1. MOA: Irritate gastric mucosa and stimulate respiratory tract secretions to increase respiratory fluid volumes and decrease mucous viscosity.
1.4.3.2. Clinical Use: Expectorant, cystic fibrosis?
1.4.3.3. Problems: few
