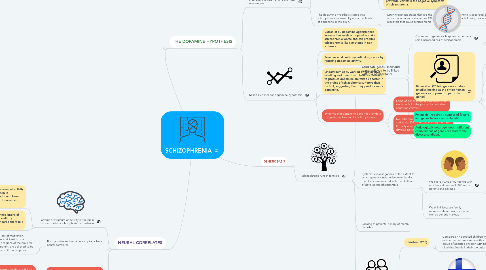
1. THE DOPAMINE HYPOTHESIS
1.1. Neurotransmitters - brain's chemical messengers
1.1.1. Appear to work differently in the brain of a patient with schizophrenia.
1.1.1.1. Dopamine is widely believed to be involved.
1.1.1.1.1. Important in the functioning of several brain systems that may be implicated in the symptoms of schizophrenia.
1.1.1.2. Hyperdopaminergia - subcortex - the possible role of high levels of activity of dopamine in the subcortex.
1.1.1.2.1. The excess of dopamine receptors in Bronca's area may be associated with poverty of speech and/or the experience of auditory hallucinations.
1.1.1.3. Hypodopaminergia - cortex - Goldman-Rakic et al. (2004) have identified a role for low levels of dopamine in the prefrontal cortex in the negative symptoms of schizophrenia.
1.1.2. The dopamine hypothesis states that schizophrenia is caused by abnormal levels of dopamine in the brain.
1.1.2.1. Later hypothesis states that it is the abnormal number of dopamine (D2) receptors that cause schizophrenia.
1.1.2.1.1. More dopamine is absorbed and passed along instead of being reabsorbed or lost.
1.2. Mixed evidence for dopamine hypothesis
1.2.1. Curran et al. dopamine agonists that increase the levels of dopamine make schizophrenia worse and can produce schizophrenia-like symptoms in non sufferers.
1.2.2. Tauscher et al. anti-psychotic drugs work by reducing dopamine activity.
1.2.3. Lindostroem et al. worked on radioactive labelling and found that chemicals needed to produce dopamine are taken up faster in the brains of schizophrenia sufferers than control, suggesting that they produce more dopamine.
1.2.4. Evidence that dopamine does not provide a complete explanation for schizophrenia.
1.2.4.1. Some of genes identified by Ripke et al. study code for the production of other neurotransmitters.
1.2.4.2. Neurotransmitter glutamate (Moghaddam and Javitt 2012) - dopamine might not be the only neurotransmitter that is a factor of developing schizophrenia.
2. NEURAL CORRELATES
2.1. Patterns of structure or activity in the brain that occur with a schizophrenic experience
2.1.1. Jackel et al. (2006) have measured activity levels in the ventral striatum in schizophrenia patients and found lower activity levels than those observed in controls.
2.1.1.1. Observed a negative correlation between the activity levels and the severity of overall negative symptoms. (Ventral striatum is a neural correlate of negative symptoms of schizophrenia.
2.1.2. Allen et al. (2007) scanned brains of patients experiencing auditory hallucinations and compared them to a control group.
2.1.2.1. Lower activation levels in the superior temporal gyrus and anterior cingulate gyrus were found in the hallucination group, who made more errors than the control group.
2.1.2.1.1. Reduced activity in these two areas of the brain is a neural correlate of auditory hallucinations.
2.2. Both positive and negative symptoms have neural correlates.
2.2.1. Avolition involves loss of motivation. Motivation involves anticipation of a reward, and certain regions of the brain for example ventral stratum, are believed to be particularly involved in this anticipation
2.2.1.1. Abnormality of areas like ventral stratum may be involved in the development of avolition.
2.3. There are other possible explanations for the correlation
2.3.1. e.g. correlation between levels of activity in the ventral striatum and negative symptoms of schizophrenia.
2.3.1.1. May be that there is something wrong in the stratum that is causing negative symptoms.
2.3.1.1.1. Just as possible that the negative symptoms themselves mean that less information passes through stratum,
2.3.1.1.2. May be another factor influences both the negative symptoms and the ventral striatum activity.
2.4. Tells us relatively little in itself.
3. GENETIC BASIS
3.1. Schizophrenia runs in families
3.1.1. Candidate genes - individual genes believed to be linked with risk of inheritance
3.1.1.1. A number of genes each appear to confer a small increased risk of schizophrenia.
3.1.1.1.1. Genes associated with increased risk included those coding for the functioning of a number of neurotransmitters including dopamine.
3.1.1.2. Ripke et al. (2014) - genome studies (studies looking at the entire human genome as opposed to particular genes)
3.1.1.2.1. Compared the genetic makeup of 37000 patients that had schizophrenia to 113000 controls to find candidate genes that cause schizophrenia.
3.1.1.2.2. Supports the biological explanation of schizophrenia.
3.1.1.2.3. Too many combinations, therefore it is difficult to test for it and predict if someone has schizophrenia.
3.1.1.2.4. Limited implication
3.1.1.3. Polygenic - requires a number of factors and genes to work in combination.
3.1.1.4. Aetiologically heterogeneous - different combinations of genes can lead to the disease/condition.
3.1.2. Systematic investigations of the extent to which genetic similarity between family members is associated with the likelihood of developing schizophrenia
3.1.2.1. We share 100% of our genes with an identical twin and 50% with a parents and siblings.
3.1.2.1.1. Gottesman et al. (1991) large-scale family study
3.1.2.2. Weak link because family members share environment as well as genetic makeup
3.1.3. Looking at patients' history of mental disorders
3.1.4. Adoption studies
3.1.4.1. Henston (1966)
3.1.4.1.1. Compared 47 adopted children whose mother had schizophrenia with a control group of adopted children with no history of schizophrenia in their biological family.
3.1.4.2. Tienari et al. (2004)
3.1.4.2.1. Finland
3.1.4.3. Suggests that there is a genetic basis for schizophrenia - genes that make us more vulnerable to the disorder might be inherited.

