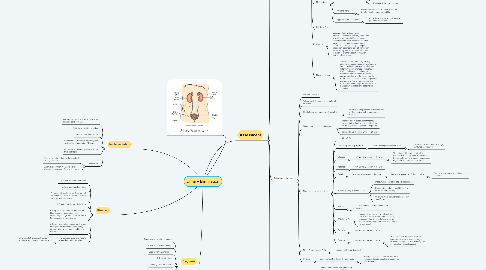
1. Urinary System
2. Diagnosis
2.1. Functional urinary incontinence
2.2. Stress urinary incontinence
2.3. Urge urinary incontinence
2.4. Risk for infection
2.5. Toileting self-care deficit
2.6. Impaired skin integrity
2.7. Impaired urinary elimination
2.8. Urinary retention
3. Planning
3.1. 1. Maintain adequate hydration.
3.2. 2. Keep good voiding habits
3.3. 3. Keep the bowels regular. A rectum full of stool may irritate the bladder, causing urgency and frequency.
3.4. 4. Prevent urinary tract infections.
3.5. 5. Stop smoking to reduce your risk for bladder cancer and reduce risk of developing a cough which can contribute to stress urinary incontinence.
3.6. 6. Report to your health care provider any changes in bladder habits, frequency, urgency, pain when voiding, or blood in the urine.
3.7. 7. Encourage kegel exercises to strengthen pelvic muscles
3.7.1. Pelvic muscle training is effective in treating stress urinary incontinence
4. Implementation
4.1. Females should wipe front to back when cleaning perineum area
4.2. Establish a toileting schedule
4.3. Provide incontinence care
4.4. Monitor Intake/Output every shift, view the trend over a period of 24 hours
4.5. Increase Fluid Intake if patient is not on fluid restriction
4.6. Medication
4.6.1. Finish all antibiotic therapy if prescribed for any infection
4.6.2. Anemia is common in chronic kidney disease, manage with Fe, erythropoetin
5. Assessment
5.1. Normal Urine Elimination (Micturition)
5.1.1. 50-60 mL/hr (30 mL /hr)
5.1.1.1. *if it's less than 30mL/hr it's a concern
5.1.2. I/O = over 24 hr period
5.1.3. Color: pale yellow, clear
5.1.4. No pain
5.1.5. No blood
5.1.6. No protein
5.1.7. No urgency
5.1.8. No foul odor, urine has ammonia smell
5.1.9. Physical Assessment
5.1.9.1. no tenderness over the symphysis pubis
5.2. Factors Affecting Urinary Elimination
5.2.1. Age
5.2.1.1. Children: Can control voiding 18 to 24 months
5.2.1.2. Gravity + childbirth weaken the pelvic floor
5.2.1.3. Prostate can enlarge in older males, it can obstruct the bladder outlet and cause urinary retention + urgency
5.2.1.4. Older Adult
5.2.1.4.1. Fewer nephrons
5.2.1.4.2. Loss of muscle tone of the bladder
5.2.1.4.3. Can't empty bladder effectively
5.2.1.4.4. Increase Nocturia
5.2.2. Psychosocial Factors
5.2.2.1. Emotional Stress and Anxiety
5.2.2.1.1. increases the frequency of urinating
5.2.2.2. Lack of privacy in hospitals
5.2.2.3. Not having enough breaks/time to urinate
5.2.3. Pain
5.2.3.1. Pain in the urinary tract, person may suppress the urge to urinate
5.2.3.2. obstructions in the ureter
5.2.4. Fluid Intake
5.2.4.1. increased fluid intake increases urine production
5.2.4.2. Caffeine
5.2.4.2.1. Fluids containing caffeine and other bladder irritants can prompt unsolicited bladder contractions resulting in frequency, urgency, and incontinence.
5.2.5. Pathological Conditions
5.2.5.1. Diabetes mellitus, multiple sclerosis, and stoke can alter bladder contractility in addition to the ability to sense bladder filling. Patients will experience either bladder overactivity or deficient bladder emptying.
5.2.5.2. Arthritis, Parkinson’s disease, dementia, and chronic pain syndromes can interfere with timely access to a toilet.
5.2.5.3. Spinal cord injury or intervertebral disk disease (above S-1) can cause the loss of urine control due to bladder overactivity and impaired coordination between the contracting bladder and urinary sphincter.
5.2.6. Surgical Procedures
5.2.6.1. Local trauma during lower abdominal and pelvic surgery sometimes obstructs urine flow requiring temporary use of an indwelling urinary catheter.
5.2.6.2. Anesthetic agents and other agents given during surgery can decrease bladder contractility and/or sensation of bladder fullness causing urinary retention
5.2.7. Medications
5.2.7.1. Diuretics increase urinary output by preventing reabsorption of water and certain electrolytes.
5.2.7.2. Can Change the color of urine
5.2.7.2.1. ex. pyridium commonly used in concurrent tx with UTIs
5.2.7.2.2. Riboflavin: bright yellow urine
5.2.7.3. Aniticholinergics
5.2.7.3.1. may increase the risk for urinary retention by inhibiting bladder contractility
5.2.7.4. Hypnotics and sedatives
5.2.7.4.1. reduce the ability to recognize and act upon the urge to void.
5.2.8. Self Care Ability
5.2.9. Culture
5.2.9.1. Be aware of cultural and gender differences related to the very private act of voiding and how it affects nursing assessment and care. Be sensitive and ask questions in a straightforward manner. Culture will often dictate gender specific roles when it comes to care of elimination issues. It may be inappropriate for a male to touch or even talk about elimination matters with a woman.
5.2.10. Nursing History
5.2.10.1. Ask the patient about daily voiding patterns, including frequency and times of day, normal volume at each voiding, and history of recent changes. Frequency of voiding varies among individuals depending on fluid intake, medications such as diuretics and the use of bladder irritants such as caffeine. Most people void an average of five or more times a day. Information about the pattern of urination is necessary to establish a baseline for comparison.
5.3. Labs/Diagnostic Tests
5.3.1. Random urinalysis
5.3.2. “Clean-catch”/midstream for culture & sensitivity
5.3.3. Sterile Specimen for culture & sensitivity
5.3.3.1. Determines the presence of bacteria and to which antibiotic the bacteria are sensitive
5.3.4. Timed urine (2, 12, 24 collections)
5.3.4.1. Measure bodily substances that may be excreted at higher levels at specific times of the day or over a specific time period
5.3.4.2. discard 1st void, collect urine for 24 hours
5.3.5. Normal Lab values Urinalysis
5.3.5.1. pH (4.6 to 8.0)
5.3.5.2. Protein (up to 8 mg/100 mL)
5.3.5.2.1. Not normally present in the urine
5.3.5.3. Glucose
5.3.5.3.1. Not normally present in the urine
5.3.5.4. Ketones
5.3.5.4.1. Not normally present in the urine
5.3.5.5. Blood
5.3.5.5.1. Not normally present in the urine
5.3.5.6. Specific gravity 1.0053 to 1.030
5.3.5.6.1. measure concentration of particles in urine
5.3.5.6.2. Dehydration, reduced renal blood flow, elevate specific gravity.
5.3.5.6.3. Overhydration, early renal disease, reduce specific gravity
5.3.5.7. WBC's
5.3.5.7.1. Elevated numbers indicate inflammation or infection.
5.3.5.8. RBC (up to 2)
5.3.5.8.1. Damage to glomeruli or tubules allows RBCs to enter the urine. Trauma, disease, presence of urethral catheters, or surgery of the lower urinary tract also causes RBCs to be present.
5.3.5.9. Bacteria
5.3.5.9.1. Not normally present in urine
5.3.5.10. Crystals
5.3.5.10.1. Not normally present in urine
5.3.6. Blood Creatinine and BUN
5.3.6.1. elevated with renal dysfunction
5.3.7. CT Scan
5.3.7.1. inject contrast and view the structures
5.3.7.1.1. Identify anatomical abnormalities, renal tumors and cysts, calculi, and obstruction of the ureters
5.4. Complications
5.4.1. Kidney disease
5.4.1.1. The most common urinary elimination problems involve the inability to store urine or to fully empty urine from the bladder. Problems can result from infection, irritable or overactive bladder, obstruction of urine flow, impaired bladder contractility, or issues that impair innervation to the bladder resulting in sensory or motor dysfunction.
5.4.1.2. Chronic kidney disease
5.4.1.2.1. prone to anemia because Erythropoietin, produced by the kidneys, stimulates red blood cell production
5.4.2. Urinary Retention
5.4.2.1. the inability to partially or completely empty the bladder.
5.4.2.2. Bladder Scan
5.4.2.2.1. foley catheter/straight catheter
5.4.2.3. Incontinence
5.4.2.3.1. Incontinence caused by urinary retention is called overflow incontinence or incontinence associated with chronic retention of urine. The pressure in the bladder exceeds the ability of the sphincter to prevent the passage of urine and the patient will dribble urine.
5.4.3. Urinary Tract Infection
5.4.4. Urinary Diversion
5.4.4.1. Urinary diversions are constructed from a section of intestine to create a storage reservoir or conduit for urine. Diversions can be temporary or permanent, continent or incontinent.
5.4.4.2. A. continent urinary reservoir
5.4.4.3. B. Urostomy (ileal conduit)
5.4.4.3.1. patient has no sensation or control over the continuous flow of urine through the ileal conduit, requiring the effluent (drainage) to be collected in a pouch.
5.4.5. Urinary Diversions
5.4.6. Nephrostomy tubes
5.4.6.1. Nephrostomy tubes are small tubes that are tunneled through the skin into the renal pelvis. These tubes are placed to drain the renal pelvis when the ureter is obstructed. Patients do go home with these tubes and need careful teaching about site care and signs of infection.
