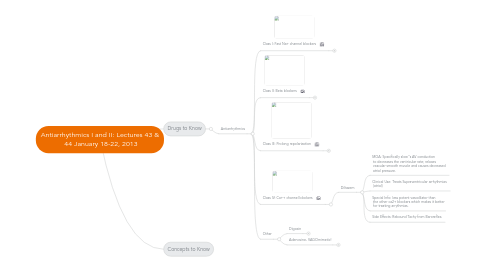
1. Drugs to Know
1.1. Antiarrhythmics
1.1.1. Class I: Fast Na+ channel blockers
1.1.1.1. IA- Intermediate Rate of Dissociation
1.1.1.1.1. Quinidine- not with DIGOXIN
1.1.1.1.2. PROcainamide- PRO Arrhythmic
1.1.1.2. IB- Very Quick Dissociation
1.1.1.2.1. Lidocaine - only class I drug WITHOUT some potassium channel blockage
1.1.1.3. IC- Very Slow Dissociation
1.1.1.3.1. Flecainide- can't use on hearts with structural defects!!!
1.1.2. Class II: Beta blockers
1.1.2.1. Propanolol
1.1.2.1.1. MOA: competitive antagonist at beta adrenergic receptors
1.1.2.1.2. Clinical Use: supraventricular tachyarrhythmias and atrial and ventricular arrhythmias prevents sudden cardiac death in post MI pts.
1.1.2.1.3. Special Info: 1st line for angina, it slows the AV node conduction in arrh. standard of care post-MI, NOT first line for HTN.
1.1.2.1.4. Effects on arrhythmia: decrease heart rate and ectopic automaticity. also enhance AV block, reduce contractility and oxygen demand.
1.1.2.2. Metoprolol
1.1.2.2.1. MOA: competitive antagonist at beta1 adrenergic receptors (specifically beta1 blockade)
1.1.2.2.2. Clinical Use: supraventricular tachyarrhythmias and atrial and ventricular arrhythmias prevents sudden cardiac death in post MI pts.
1.1.2.2.3. Special Info: Metoprolol blocks beta 1 which is almost exclusively expressed in the heart; therefore, it has cardioselectivity!
1.1.2.2.4. Effects on arrhythmia: decrease heart rate and ectopic automaticity. also enhance AV block, reduce contractility and oxygen demand.
1.1.2.3. Esmolol- short acting degraded by esterases
1.1.2.3.1. MOA: competitive antagonist at beta adrenergic receptors
1.1.2.3.2. Clinical Use: supraventricular tachyarrhythmias and atrial and ventricular arrhythmias prevents sudden cardiac death in post MI pts.
1.1.2.3.3. Effects on arrhythmia: decrease heart rate and ectopic automaticity. also enhance AV block, reduce contractility and oxygen demand.
1.1.3. Class III: Prolong repolarization
1.1.3.1. Amiodarone- blocks all channels - Na+, Ca2+, K+, Beta adrenergic
1.1.3.1.1. Clinical Use: all purpose-antiarrh. used in ventricular tachycardia (resistant to other therapies) and atrial tachyarrh.
1.1.3.1.2. MOA: Primarly blocks potassium channels thereby prolonging action potential duration!
1.1.3.1.3. Special Info: decreases slope of phase 4 depolarization in the sinus node and lowers AV-conduction (Ca2+ block), and lowers Vmax of fast response Action Potentials. (Na+ block).
1.1.3.1.4. Side effects: No real effects in the short term. BUT the LONG TERM- can get fatal pulmonary fibrosis and liver damage.
1.1.4. Class IV: Ca++ channel blockers
1.1.4.1. Diltazem
1.1.4.1.1. MOA: Specifically slow''s AV conduction to decreases the ventricular rate; relaxes vascular smooth muscle and causes decreased atrial pressure.
1.1.4.1.2. Clinical Use: Treats Supraventricular arrhythmias (atrial)
1.1.4.1.3. Special Info: less potent vasodilator than the other ca2+ blockers which makes it better for treating arrythmias.
1.1.4.1.4. Side Effects: Rebound Tachy from Baroreflex.
1.1.5. Other
1.1.5.1. Digoxin
1.1.5.1.1. MOA: specifically inhibits the Na+/K+ pump in cardiac muscle, this slows conduction and increases the refractory period. also depolarizes baroreceptor nerve endings.
1.1.5.1.2. Special Info: Increases the parasympathetic activity which further slows the HR! destributed to the body fat. PO, IV, narrow therapeutic index, Interacts with Quinidine and Diuretics
1.1.5.1.3. Side effects: Cardiac arrhythmia( Av block, ventricular tachyarrhythmia), GI distress *vomiting, nausea, diarrhea), Neurological issues (blurred vision, halos, etc.)
1.1.5.1.4. Clinical Use: treats atrial fibrillation and heart failure
1.1.5.2. Adenosine- VAGOmimetic!
1.1.5.2.1. MOA: Acts through G-protein coupled receptors to decreases automaticity and inhibit sympathetic effects (vagomimetic); slows AV conduction, and inhibits DADs
1.1.5.2.2. Clinical Use: Conversion of paroxysmal supraventricular tachycardia to sinus rhythm. (This will actually stop the heart temporarily!)
1.1.5.2.3. Special Info: This is give IV, and we watch the ECG and wait for a flat line and restart. The half life is extremely short (only seconds long)
1.1.5.2.4. Side effects: increased DADs (delayed afterdepolorizations), complete heart block, ventricular arrhythmia.
