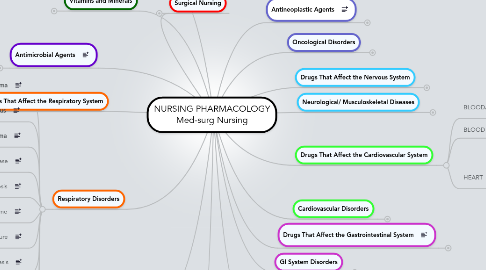
1. Drugs That Affect the Respiratory System
1.1. ANTITUSSIVES
1.1.1. Opioids
1.1.2. Nonopioids
1.2. EXPECTORANTS
1.3. DECONGESTANTS
1.3.1. Common Sympathomimetics
1.3.2. Corticosteroids
1.4. MUCOLYTICS
1.5. ANTIHISTAMINES
1.6. CORTICOSTEROIDS
1.7. BRONCHODILATORS
1.7.1. Beta Adrenergics
1.7.2. Anticholinergics
1.7.3. Xanthine Derivatives
1.7.4. Leukotriene Modifiers
1.7.5. Mast Cell Stabilizers
2. Antimicrobial Agents
2.1. ANTIBACTERIAL AGENTS
2.1.1. Penicillins
2.1.2. Cephalosporins
2.1.3. Aminogylcosides
2.1.4. Fluoroquinolones
2.1.5. Macrolides
2.1.6. Tetracyclines
2.1.7. Sulphonamides
2.2. ANTIVIRAL AGENTS
2.3. ANTITUBERCULAR AGENTS
2.4. ANTIFUNGAL AGENTS
2.5. ANTIPROTOZOAL AGENTS/ ANTIMALARIALS
2.6. ANTHELMINTIC AGENTS
2.7. ANTISEPTICS AND DISINFECTANTS
3. Drugs That Affect the Urinary System
3.1. DIURETICS
3.1.1. Carbonic Anhydrase Inhibitors
3.1.2. Loop Diuretics
3.1.3. Osmotic Diuretics
3.1.4. Potassium-Sparing Diuretics
3.1.5. Thiazides and Thiazidelike Diuetics
3.2. URINARY ANAESTHETICS
3.3. SMOOTH MUSCULAR STIMULANTS (CHOLINERGICS)
4. Vitamins and Minerals
4.1. VITAMINS
4.1.1. FAT-SOLUBLE VITAMINS
4.1.1.1. A
4.1.1.2. D
4.1.1.3. E
4.1.1.4. K
4.1.2. WATER-SOLUBLE VITAMINS
4.1.2.1. B Complex
4.1.2.2. C
4.2. COMMON MINERALS
4.2.1. Iron
4.2.2. Calcium
4.2.3. Phosphorus
4.2.4. Magnesium
4.2.5. Sodium
4.2.6. Potassium
4.2.7. Zinc
5. Respiratory Disorders
5.1. Asthma
5.2. Pulmonary Embolus
5.3. Pulmonary Edema
5.4. Chronic Obstructive Pulmonary Disease
5.5. Tuberculosis
5.6. Acute Respiratory Distress Syndrome
5.7. Acute Respiratory Failure
5.8. Atelectasis
5.9. Pneumothorax
5.10. Lung Cancer
6. Renal Disorders
6.1. Urinary Tract Infections
6.2. Pyelonephritis
6.3. Nephrotic Syndrome
6.4. Glomerulonephritis
6.5. Urinary Tract Calculi
6.6. Polycystic Kidney Disease
6.7. Acute Renal Failure
6.8. Chronic Renal Failure
6.9. Dialysis
7. Endocrine Disorders
7.1. Type 1 Diabetes
7.2. Type 2 Diabetes
7.3. Diabetes Isipidus
7.4. Syndrome of Inappropriate Antidiuretic Hormone
7.5. Addison's Disease
7.6. Cushing's Syndrome
8. Surgical Nursing
8.1. Pre-Op work up
8.2. Post-Op Complications/Care
8.3. Bowel Obstructions
9. GI System Disorders
9.1. Peptic Ulcer Disease
9.2. Gastroesophageal Reflux (GERD)
9.3. Gastritis
9.4. Appendicitis
9.5. Diverticulitis
9.6. Inflammatory Bowel Disease
9.7. Ulcerative Colitis
9.8. Crohn's Disease
9.9. Colorectal Cancer
9.10. Jaundice
9.11. Cholelithiasis
9.12. Hepatitis
9.13. Cirrhosis
9.14. Pancreatitis
10. Drugs That Affect the Nervous System
10.1. Central Nervous System
10.1.1. DEPRESSANTS
10.1.1.1. Analgesics - Opioids
10.1.1.1.1. Opioid Antagonists
10.1.1.1.2. Nonopioids
10.1.1.2. Sedatives, Hypnotics, Anxiolytic Agents
10.1.1.2.1. Barbiturates
10.1.1.2.2. Benzodiazepines
10.1.1.2.3. NonBenzodiazepines
10.1.1.3. Antiseizure Agents
10.1.1.3.1. Barbiturates
10.1.1.3.2. Benzodiazepines
10.1.1.3.3. Hydantoins
10.1.1.3.4. Carbamazepines
10.1.1.3.5. Valproic Acid
10.1.1.4. Anti-Parkinson Drugs
10.1.1.4.1. Dopaminergics
10.1.1.4.2. Anticholinergics
10.1.1.5. Skeletal Muscle Relaxants
10.1.2. Psychotropic Drugs
10.1.2.1. Antidepressants
10.1.2.2. Mood Stabilizers
10.1.2.3. Antipsychotics
10.1.3. Anaesthetics
10.1.3.1. Locally Acting
10.1.3.2. General (Systemic)
10.1.3.3. Neuromuscular Blocking Agents
10.1.4. Stimulants
10.1.4.1. Amphetamines
10.2. Autonomic Nervous System
10.2.1. SYMPATHETIC DIVISION
10.2.1.1. Adrenergics
10.2.1.2. Antiadrenergics or Adrenergic Blocking Agents
10.2.2. PARASYMPATHETIC DIVISION
10.2.2.1. Cholinergics
10.2.2.2. Anticholinergics
11. Drugs That Affect the Cardiovascular System
11.1. BLOOD/COAGULATION
11.1.1. Anticoagulants
11.1.1.1. Heparin
11.1.1.2. Warfarin
11.1.1.3. Antiplatelet Drugs
11.1.2. Fibrinolytics
11.1.3. Antilipemics
11.1.4. Antianemics
11.2. BLOOD VESSELS
11.2.1. Antihypotensives
11.2.2. Antihypertensives
11.3. HEART
11.3.1. Cardiotonics (Inotropics)
11.3.2. Antidysrhythmics
11.3.3. Anti-Angina Pectoris Drugs
12. Drugs That Affect the Gastrointestinal System
12.1. LAXATIVES
12.1.1. Bulk Forming
12.1.2. Emollient
12.1.3. Stimulant
12.1.4. Hyperosmotic
12.2. ANTIDIARRHEALS
12.2.1. Opioids
12.2.2. Bulk Forming
12.2.3. Absorbents
12.2.4. Anticholinergics
12.3. ANTACIDS
12.3.1. Neutralizing Agents
12.3.2. H2 Receptor Antagonists
12.3.3. Proton Pump Inhibitors
12.3.4. Muscosal Protective Agents
12.4. ANTIEMETICS
12.4.1. Anticholinergics
12.4.2. Antihistamines
12.4.3. Neuroleptics
12.4.4. Prokinetics
12.4.5. Serotonin Blockers
12.4.6. Cannabis
13. Antineoplastic Agents
13.1. Alkylating Agents
13.2. Antimetabolites
13.3. Mitotic Inhibitors
13.4. Antitumor Antibiotics
13.5. Topoisomerase-1 Inhibitors
13.6. Hormonal Antagonists
13.7. Biological Response Modifiers
14. Cardiovascular Disorders
14.1. Brain Attack - TIA
14.2. Hypertension
14.3. Coronary Artery Disease (CAD)
14.3.1. Angina
14.3.2. Myocardial Infarction (MI)
14.3.3. Sudden Cardiac Death
14.4. Valvular Heart Disease
14.5. Dysrhythmias
14.6. Peripheral Vascular Disease
14.7. Abdominal Aortic Aneurysm (AAA)
14.8. Heart Failure
14.9. Shock
14.9.1. Anaphylactic
14.9.2. Cardiogenic
14.9.3. Septic
14.10. Hypovolemia
14.11. Cardiopulmonary Arrest
15. Neurological/ Musculoskeletal Diseases
15.1. Multiple Sclerosis (MS)
15.2. Parkinson's Disease
15.3. Spinal Cord Injury
15.4. Osteomyelitis
15.5. Osteoporosis
15.6. Fibromyalgia Syndrome
15.7. Chronic Fatigue Syndrome
15.8. Osteoarthritis
15.9. Rheumatoid Arthritis
15.10. Systemic Lupus Erythematosus
15.11. Trauma, Burns, Fractures
15.12. Head Injury
15.12.1. Subarachnoid Hemorrhage
