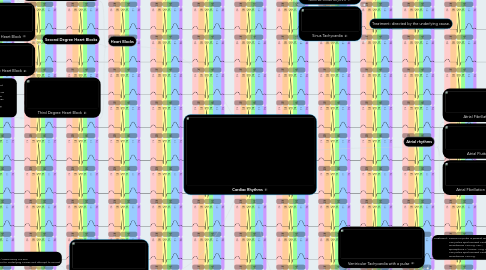
1. Asystole/PEA
1.1. Treatment: CPR epinephrine 1/10000 every 3-5 min assess H's & T's for underlying causes and attempt to correct
2. Heart Blocks
2.1. First Degree Heart Block
2.1.1. Treatment: usually not needed. consider O2, IV with atropine 0.5 mg. x3, transcutaneous pacing, and a dopamine drip to treatment any complications. Avoid drugs that slow AV conduction, like lidocaine and procainamide, if possible
2.2. Second Degree Heart Blocks
2.2.1. Type I Second Degree Heart Block
2.2.1.1. Treatment; usually not needed except monitoring. If heart rate falls and patient become symptomatic, administer 0.5 mg. of atropine via IV every 3-5 min. until heart rate improves or a max of 3.0 mg. has been given. If atropine fails, consider transcutaneous pacing or a dopamine or epinephrine drip.
2.2.2. Type II Second Degree Heart Block
2.2.2.1. Treatment; usually not needed except when signs of poor perfusion is present. If signs of poor perfusion are present, consider 0.5 mg. of atropine sulfate via bolus every 3-5 min. until heart rate improves or a max of 3.0 mg. has been given. If atropine fails, consider transcutaneous pacing or a dopamine or epinephrine drip.
2.3. Third Degree Heart Block
2.3.1. Treatment; usually not needed except monitoring. If heart rate falls and patient become symptomatic, administer 0.5 mg. of atropine via IV every 3-5 min. until heart rate improves or a max of 3.0 mg. has been given. If atropine fails, consider transcutaneous pacing or a dopamine or epinephrine drip.
3. Sinus Rhythms
3.1. Sinus Bradycardia
3.1.1. Treatment; usually not needed unless signs of poor perfusion are present. if poor perfusion is present, administer 0.5 mg. of atropine via IV bolus every 3-5 min. for a max of 3.0 mg If atropine fails, consider transcutaneous pacing or a dopamine or epinephrine drip.
3.2. Normal Sinus Rhythm
3.2.1. Treatment: none needed. this is what a normal cardiac rhythm looks like
3.3. Sinus Tachycardia
3.3.1. Treatment: directed by the underlying cause.
4. Atrial rhythms
4.1. Atrial Fibrillation
4.1.1. Treatment for stable: O2 Cardizem 20 mg. slow IV push over 5 min. 50 joules synchronized cardioversion Treatment for unstable: O2 50 joules synchronized cardioversion Cardizem 20 mg. slow IV push over 5 min.
4.2. Atrial Flutter
4.2.1. Treatment: same as for atrial fibrillation
4.3. Atrial Fibrillation with RVR
4.3.1. Treatment: same as for atrial fibrillation
5. Ventricular Rhythms
5.1. Ventricular Tachycardia with a pulse
5.1.1. Treatment: ensure no pulse is present and CPR is not needed 100 joules synchronized cardioversion amiodarone 150 mg. via IV epinephrine 1/10,000 1 mg. every 3-5 min. 100 joules synchronized cardioversion amiodarone 150 mg.
5.2. Ventricular Fibrillation
5.2.1. Treatment: CPR 200 joules defibrillation amiodarone 300 mg. via IV epinephrine 1/10,000 1 mg. every 3-5 min. continue CPR 200 joules defibrillation amiodarone 150 mg.
5.3. Ventricular Tachycardia without a pulse
5.3.1. Treatment: same as ventricular fibrillation
