1. Symptom
1.1. Fatigue
1.2. Nursing Assessment
1.2.1. How is appetite/food intake?
1.2.2. Does it affect your ADL's?
1.2.3. Vital Signs, BP, HR
1.2.4. Onset
1.2.5. Hemoglobin, Creatinine, Urea
1.3. Diagnostic
1.3.1. Blood work: hemoglobin, creatinine, urea, GFR
1.4. Nursing Diagnosis
1.4.1. At risk for falls as evidenced by fatigue and weakness secondary to low blood pressure, low hemoglobin and high levels of uremic toxins in blood
1.5. Intervention
1.5.1. High caloric diet, increase fat, restrict dietary protein and potassium intake
1.5.2. Promote rest, activity as tolerated
1.5.3. Erythropoietin
1.5.4. Educate on safe transfers and ambulation
1.6. Evaluation
1.7. Increased energy levels to complete ADL's
1.8. Energy levels returning to baseline
2. Symptom
2.1. Chest Pain
2.2. Nursing Assessment
2.2.1. Pain scale, location, quality, triggers (ie., exertion), onset
2.2.2. Vital signs, HR and Rhythm
2.2.3. History of Chest pain
2.3. Diagnostic
2.3.1. Troponin, Calcium, Potassium, Sodium, ECG
2.4. Nursing Diagnosis
2.4.1. Potential complication: dysrhythmias related to electrolyte disturbance
2.5. Intervention
2.5.1. Close VS monitoring, Oxygen, Nitroglycerin, Telemetry
2.6. Evaluation
2.6.1. No chest pain
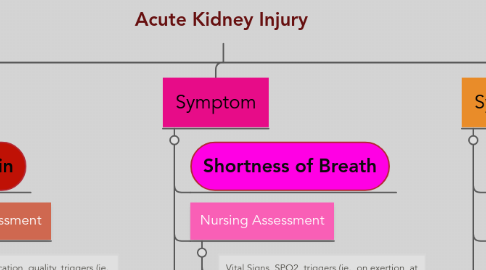
3. Symptom
3.1. Shortness of Breath
3.2. Nursing Assessment
3.2.1. Vital Signs, SPO2, triggers (ie., on exertion, at rest), physical appearance, onset
3.2.2. Chest Auscaltation: wheeze, crackles, rub
3.3. Nursing Diagnosis
3.3.1. Excess fluid volume secondary to Acute Kidney Injury and fluid retention
3.4. Intervention
3.4.1. Monitor oxygen saturation, oxygen as tolerated
3.4.1.1. Diuretic therapy ie., Furosemide
3.4.1.2. Encourage deep breathing and coughing as tolerated
3.4.1.3. Promote balanced activity and rest
3.4.1.4. Fluid restriction
3.5. Evaluation
3.5.1. No shortness of breath and distress to be noted
3.5.2. Normal oxygen saturation levels
3.5.3. Ease in performing ADL's
4. Symptom
4.1. Peripheral Edema
4.2. Nursing Assessment
4.2.1. Onset
4.2.2. Pitting or non-pitting? Duration of pitting
4.2.3. Location of edema
4.3. Nursing Diagnosis
4.3.1. Fluid retention secondary to Acute Kidney Injury as evidenced by peripheral edema to bilateral ankles and feet
4.4. Intervention
4.4.1. Encourage to elevate legs when in bed, and as tolerated
4.4.2. Daily weights: same scale, same method
4.4.3. Encourage ambulation
4.4.4. Diuretic therapy ie, Furosemide
4.4.5. Restrict dietary salt intake; PO fluid restriction
4.5. Evaluation
4.6. No peripheral edema noted
5. Symptom
5.1. Decreased Urine Output
5.2. Nursing Assessment
5.2.1. Onset
5.2.2. Urine output measurement
5.2.3. Presence of pain with urination
5.2.4. Hematuria
5.3. Diagnostics
5.3.1. Blood Work: Lytes, Creatinine, GFR, Serum Potassium
5.3.2. Urinalysis, 24-hour urine collection, C&S and Cell Count
5.4. Nursing Diagnosis
5.4.1. At risk for dehydration secondary to Acute Kidney Injury as evidenced by low urine output
5.5. Intervention
5.5.1. IV fluids to replenish fluids and flush Creatinine out of the system
5.5.2. Close VS, and input and output monitoring
5.5.3. Daily weights
5.6. Evaluation
5.6.1. Increased urinary output
5.6.2. Urinary output normal amount

