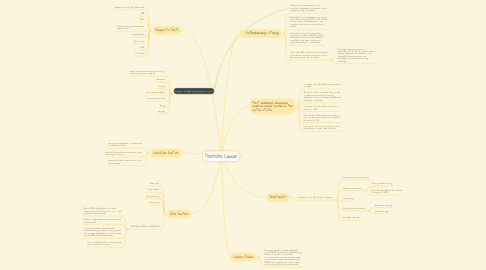
1. Common Findings with prostate cancer
1.1. Death rates have been decreasing in several countries including:
1.2. Australia
1.3. Canada
1.4. the United Kingdom
1.5. the United States
1.6. Italy
1.7. Norway
2. Causative factors
2.1. Genetic predisposition (familial and hereditary forms)
2.2. Dietary Factors (but association with obesity is unclear)
2.3. Hormones (more explanation to be determined)
3. Risk factors
3.1. Older age
3.2. Race (black)
3.3. Family History
3.4. Vasectomy
3.5. INFLAMMATION [CHRONIC]
3.5.1. Risk of BPH progression and acute urinary retention is great in men with prostatic inflammation
3.5.2. Prostatic hyperplasia is associated with inflammation
3.5.3. Certain metabolic comorbidities, including obesity, diabetes, sleep apnea, and erectile dysfunction may be linked to both BPH and inflammation
3.5.4. Chronic inflammation and prostate cancer have been linked
4. Diagnostic Tests
4.1. Blood screening with PSA levels
4.2. DRE
4.3. TRUS
4.4. Tissue biopsy and microscopic examination
4.5. Lymphography
4.6. Bone scans
4.7. MRI
4.8. CT scans
5. Pathophysiologic etiology
5.1. Prostate Cancer develops in an androgen-dependent epithelieum and is usually androgen sensitive
5.2. Androgens are synthesized not only in the testis, accounting for 50% to 60% of the total testosterone in the prostate, but also in the prostate itself
5.3. Prostate cancer cells have been reported to make androgens from cholesterol, but research involving androgens and their relation to prostate diseases in incomplete
5.4. More than 95% of prostatic neoplasms are adenocarcinomas and most occur in the periphery of the prostate
5.4.1. Prostatic adenocarcinoma is a heterogeneous group of tumors with a diverse spectrum of molecular and pathologic characteristics and therefore clinical behaviors and challenges
6. Most commonly diagnosed nonskin cancer in men in the United States.
6.1. Lifetime risk for diagnosis estimated at 15.9%
6.2. Incidence varies worldwide but is still considered 2nd most frequently diagnosed cancer and 6th leading cause of death worldwide
6.3. Lifetime risk for dying of prostate cancer is 2.8%
6.4. Rare before age 50 years, very few men die from prostate cancer before 60 years of age
6.5. More than 75% of all prostate cancer is diagnosed in men older than 65
7. Treatments
7.1. Depends on the age of the neoplasm
7.1.1. No treatment as an option
7.1.2. Surgical treatments
7.1.2.1. Total prostatectomy
7.1.2.2. Transurethral Resection of the Prostate (TURP)
7.1.3. Cryotherapy
7.1.4. Nonsurgical treatments
7.1.4.1. Radiation therapy
7.1.4.2. Chemotherapy
7.1.5. Watchful waiting

