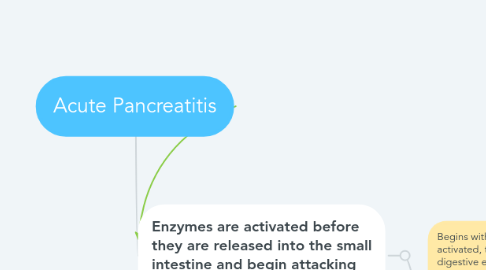
1. Enzymes are activated before they are released into the small intestine and begin attacking the pancreas.
1.1. Begins with activation of trypsin. Once activated, trypsin can activated a variety of digestive enzymes that cause pancreatic injury.
1.1.1. Pancreas becomes inflamed.
1.1.1.1. Acute Inflammatory Response
1.1.1.1.1. Cellular Stage: involves the delivery and migration of leukocytes, mainly neutrophils to the cite of injury to perform host defense. The primary function is to limit the injurious effect of the pathologic agent and remove the injured tissue. White blood cell count may be increased with acute pancreatitis which is known as leukocytosis.
1.1.1.1.2. Vascular Stage: Changes in blood vessels at the site of the injury beginning with vasoconstriction and rapid vasodilation. Vasodilation causes heat and redness accompanied by increased vascular permeability with protein-rich fluid in the extravascular spaces. Accumulation of fluid in the tissue causes swelling and pain, as fluid moves out of the vessels, flow and clotting of blood occurs which causes the swelling in acute inflammation.
1.1.1.2. Local Manifestation
1.1.1.2.1. Abdominal tenderness and distention occurs with acute pancreatitis. The accumulation of fluid from the vascular stage in tissue causes swelling and pain which is caused by the increased vascular permeability.
1.1.1.2.2. Irritation of the pancreas from inflammation can cause nausea and vomiting.
1.1.1.3. Systemic Manifestation
1.1.1.3.1. White blood cell count may be increased with acute pancreatitis which is known as leukocytosis. In an acute inflammatory response, neutrophils are the first line of defense. When the body needs to produce more neutrophils in order to compensate for inflammation, the white blood cell count increases.
1.1.1.3.2. Fevers can also occur in acute pancreatitis. Fevers are an elevation in body temperature caused by an upward displacement of the set point of the thermoregulatory center. Fevers are one of the most prominent manifestations of the acute-phase response.
1.1.1.3.3. During the acute phase response, the liver dramatically increases proteins such as the C-reactive protein. This level rises when there is an acute-inflammatory response which is seen in acute pancreatitis.
1.1.1.3.4. Acute-phase response occur during the inflammatory process. Tachycardia is common with acute pancreatitis. Manifestation of the acute-phase response includes tachycardia due to constellation of systemic effects.
1.1.1.4. Occurence
1.1.1.4.1. 20% of person with acute pancreatitis have a severe course and 10-30% of those with severe pancreatitis die
1.1.1.5. Causes
1.1.1.5.1. 70-80% cases in the United States are caused by alcohol abuse and gallstones
1.1.1.5.2. Other causes can be due to hyperlipidemia, hypercalcemia, infections, and abdominal and surgical trauma.
1.1.1.6. Diagnosis - made when two of the three following symptoms are present:
1.1.1.6.1. Abdominal pain which is severe, located in the epigastric or left upper quadrant and may radiate to the back, chest, or flank area.
1.1.1.6.2. Serum lipase greater than three times the upper limit of normal
1.1.1.6.3. Classic signs on abdominal imaging such as CT scans and ultrasonography
1.1.1.7. Treatment
1.1.1.7.1. consists of immediate management and preventing recurrence.
1.1.1.7.2. pain relief and putting the pancreas to rest by holding food and fluids
1.1.1.7.3. If abdominal distention is present, it is treated with gastric suction to prevent further stimulation of pancreatic enzymes
1.1.1.7.4. IV fluids to replace electrolytes lost from circulation

