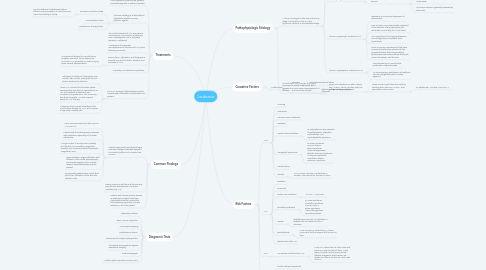
1. Treatments
1.1. Most treatment protocols use systemic chemotherapy with or without radiation.
1.2. The basic strategy is to eliminate all detectable disease by using cytotoxic agents.
1.2.1. Remission Induction Phase
1.2.1.1. Use of intrathecal methotrexate with or without cranial irradiation to cover the CNS varies from facility to facility.
1.2.2. Consolidation Phase
1.2.3. Maintenance Therapy Phase
1.3. The initial treatment of ALL uses various combinations of vincristine, prednisone, and L-asparaginase until a complete remission is obtained. Maintenance therapy with mercaptopurine is continued for 2-3 years following remission.
1.4. Daunorubicin, cytarabine, and thioguanine currently are used to obtain induction and remission of AML.
1.4.1. Maintenance therapy for 8 months may lengthen remission. Once relapse has occurred, AML generally is curable only by bone marrow transplantation.
1.5. Currently, CLL treatment is palliative.
1.6. For CML, emergent leukopheresis may be needed when leukostatic complications are present.
1.6.1. Otherwise, busulfan or hydroxyurea may control WBC counts. During the chronic phase, treatment is palliative.
1.6.2. When CML converts to the blastic phase, approximately one third of cases behave as ALL and respond to treatment with vincristine and prednisone. The remaining two thirds resemble AML but respond poorly to AML therapy.
1.6.3. Allogeneic bone marrow transplant is the only curative therapy for CML. But it carries a high early mortality rate.
2. Common Findings
2.1. Patients commonly have physical signs of anemia (fatigue, dizziness, dyspnea on exertion) pallor, and a cardiac flow murmur.
2.1.1. Fever and pneumonia can also occur in AML and ALL.
2.1.2. Patients with thrombocytopenia presents with petechiae, especially in the lower extremities.
2.1.3. A large number of ecchymoses is usually an indicator of a coexistent coagulation disorder such as disseminated intravascular coagulation (DIC).
2.1.4. Signs relating to organ infiltration with leukemic cells include splenomegaly and hepatomegaly and, to a lesser degree, lymphadenopathy may be present.
2.1.5. Occasionally, patients have rashes that result from infiltration of the skin with leukemic cells.
2.2. Rarely, a bony or soft-tissue chloroma may precede the development of marrow infiltration by AML
2.3. Patients with coronary artery disease ay experience anginal chest pain. Myocardial infarction may be the first presenting symptom of acute leukemia in an older patient.
3. Diagnostic Tests
3.1. Laboratory Studies
3.2. Bone Marrow Aspiration
3.3. Immunophenotyping
3.4. Histochemical Stains
3.5. Chromosomal Analysis/Cytogenetics
3.6. Computed Tomography/Magnetic Resonance Imaging
3.7. Chest Radiograph
3.8. Multiple gated acquisition scan(MUGA)
4. Pathophysiologic Etiology
4.1. A clone of malignant cells may arise at any stage of maturation, that is, in the lymphoid, myeloid, or pluripotential stage.
4.1.1. Acute Lymphocytic Leukemia (ALL)
4.1.1.1. A malignant clonal disorder of the bone marrow lymphopoietic precursor cells.
4.1.1.1.1. The progressive medullary and extramedullary accumulations of lymphoblasts are present that lack the potential for differentiation and maturation.
4.1.1.1.2. An inhibition of the normal development of hematopoietic cell elements occurs
4.1.2. Acute Myelogenous Leukemia (AML)
4.1.2.1. A group of neoplastic disorders of the hematopoietic precursor cells of the bone marrow
4.1.2.1.1. The time for one cell division is prolonged with respect to that of normal bone marrow blast cells.
4.1.2.1.2. Failure of maturation of the neoplastic cell clone exists.
4.1.2.1.3. The bone marrow is gradually replaced by blast cells.
4.1.3. Chronic Lymphocytic Leukemia (CLL)
4.1.3.1. represents a monoclonal expansion of lymphocytes
4.1.3.2. 95% of cases is a predominantly malignant clonal disorder of B lymphocytes; the remainder is secondary to a T-cell clone.
4.1.3.3. The neoplastic cell is a hypoproliferative, immunologically incompetent small lymphocyte.
4.1.3.4. There is primary involvement of the bone marrow and secondary release into the peripheral blood, then the circulating lymphocytes selectively infiltrate the lymph nodes, the spleen, and the liver.
4.1.4. Chronic Myelogenous Leukemia (CML)
4.1.4.1. characterized by an uncontrolled proliferation of granulocytes
4.1.4.2. An accompanying proliferation of erythroid cells and megakaryocytes is usually apparent.
4.2. In most cases, the cause for this clonal expansion is poorly understood, but it appears to involve some rearrangement of the DNA.
4.2.1. Some viral infections can alter a host's DNA or RNA, which can then push the cell toward becoming cancer
4.2.1.1. These viruses hi-jack the host's cells by inserting their own DNA or RNA, then reproduces more viruses
4.2.1.1.1. ie: Epstein-Bar Virus (EBV) and HTLV-1
5. Causative Factors
5.1. Multifactorial
5.1.1. Genetics
5.1.1.1. chromosomal abnormalities
5.1.2. Environmental Factors
5.1.2.1. alkylating drugs, ionizing radiation, chemicals
6. Risk Factors
6.1. AML
6.1.1. Smoking
6.1.2. Chemicals
6.1.3. Previous cancer treatment
6.1.4. Radiation
6.1.5. Certain blood problems
6.1.5.1. ie: polycythemia vera, essential thrombocytemia, idiopathic myelofibrosis, and myelodysplastic syndrome
6.1.6. Congenital Syndromes
6.1.6.1. ie: Down syndrome Fanconi anemia Bloom syndrome Ataxia-telangiectasia Blackfan-Diamond syndrome Li-Fraumeni syndrome Neurofibromatosis I Kostmann Syndrome
6.1.7. Family history
6.1.8. Gender
6.1.8.1. AML is more common in males than in females. The reasons for this are not clear.
6.2. ALL
6.2.1. Radiation
6.2.2. Chemicals
6.2.3. Certain viral infections
6.2.3.1. ie: HTLV-1 virus, EBV
6.2.4. Inherited Syndromes
6.2.4.1. ie: Down syndrome Klinefelter syndrome Fanconi anemia Bloom syndrome Ataxia-telangiectasia Neurofibromatosis
6.2.5. Gender
6.2.5.1. Slightly more common in males than in females, but the reason for this is unknown.
6.2.6. Race/Ethnicity
6.2.6.1. More common in whites than in African Americans, but the reasons for this are not clear.
6.2.7. Identical twin with ALL
6.3. CML
6.3.1. No proven risk factors for CML.
6.3.1.1. Most CML cases have no clear cause and there is no way to prevent them. Many types of cancer can be prevented by lifestyle changes to avoid certain risk factors, but this is not true for most cases of CML.
6.4. CLL
6.4.1. Certain chemical exposures
6.4.2. Family history
6.4.2.1. First-degree relatives have more than twice the risk for this cancer.
6.4.3. Gender
6.4.3.1. Slightly more common in males than females, but the reasons for this are not known.
6.4.4. Race/Ethnicity
6.4.4.1. More common in North America and Europe than in Asia. Most experts suggest that this is related to genetic differences rather than environmental factors because people keep the same risk even when they move from one area to another.
