1. Practitioner Dos and Don'ts
1.1. Dos
1.1.1. Be a collaborator
1.1.2. Listen
1.1.3. Be empathic
1.1.4. Separate the child from the symptoms
1.1.5. Avoid blame
1.1.6. Be willing to refer
1.2. Don'ts
1.2.1. Don't talk about the child in front of the child.
1.2.2. Don't ignore mood
1.2.3. New nodeDon't blame children for lack of treatment success
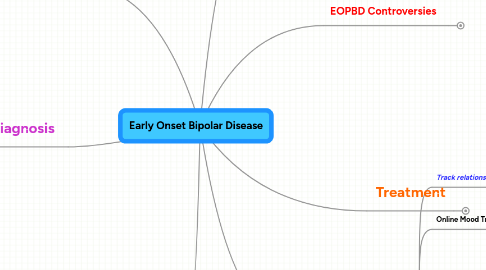
2. Diagnosis
2.1. USE MULTIPLE INFORMANTS!!
2.2. Presenting Symptoms
2.2.1. Common Presenting Symptoms in Children
2.2.1.1. Episodes of deprssed mood/hopelessness
2.2.1.2. Excessive mood lability
2.2.1.3. Periods of increased or decreased energy
2.2.1.4. episodes of decreased need for sleep
2.2.1.5. anger dyscontrol
2.2.1.6. markedly irritable moods
2.2.1.7. frequent argumentativeness
2.2.1.8. bold/intrusive/demanding behaviors
2.2.2. Adolescent Presentation
2.2.2.1. discrete episodes of mania and depression
2.2.2.2. rapid symptom onset
2.2.2.3. mood-congruent psychotic features
2.2.2.4. hospitalization more common due to severity
2.2.3. Early Onset BPD vs. Adult BPD
2.2.3.1. Less discrete episodes
2.2.3.2. often mixed states, ultrarapid cycling
2.2.3.3. sometimes cycling more then once a day (ultradian)
2.2.3.4. irritability across episodes
2.2.3.5. emotionally labile
2.2.3.6. explosive outbursts
2.3. Difficult to diagnose
2.3.1. Why?
2.3.1.1. Low base rate
2.3.1.2. Variable clinical presentation
2.3.1.3. Effects of development on presentation
2.3.1.4. High comorbidity!
2.3.1.4.1. ADHD 40-90%
2.3.1.4.2. Anxiety disorders 20-40%
2.3.1.4.3. Conduct Disorders 20 to 50%
2.3.1.4.4. ODD 20-60%
2.3.1.5. Disorder not clearly defined by the profession
2.4. Differential diagnosis
2.4.1. ADHD
2.4.1.1. persistent vs. episodic in nature
2.4.1.2. ADHD earlier onset
2.4.2. Conduct Disorder
2.4.2.1. CD usually longer standing
2.4.2.2. BPD more likely to have family history of affective disorder
2.4.3. Psychosis/Schizophrenia
2.4.3.1. Hard to differentiate during mania--need to observe closely
2.4.3.2. BPD commonly misdiagnosed as schizophrenia
2.4.3.2.1. look for family history of schizophrenia or schizotypal disorder
2.4.3.2.2. Determine premorbid symptoms
2.5. Diagnostic Instruments
2.5.1. Young Mania Rating Scale (YMRS)
2.5.1.1. Parent Version (PDF)
2.5.2. Child Mania Rating Scale (CMRS)
2.5.2.1. Parent Version (PDF)
2.5.3. K-SADS Mania Rating Scale
2.5.4. Child Behavior Checklist (CBL)
2.6. Assess for suicide!
3. Professional Articles
3.1. AAACAP Practice Parameters (PDF)
3.2. CABF Workgroup Treatment Guidelines (PDF)
3.3. Course and Outcome of Bipolar Spectrum Disorder in Children and Adults: A Review of the Literature (PDF)
3.4. Pediatric bipolar disorder: Evidence for its diagnostic validity and recommendations for making the diagnosis (PDF)
3.5. The Role of the Family in the Course and Treatment of Bipolar Disorder (PDF)
3.6. Psychosocial Interventions for Children with Early-Onset Bipolar Spectrum Disorder.
3.7. Bipolar Disorder in Childhood and Adolescence (PDF)
4. Mood Tracking
4.1. Track relationships between
4.1.1. Symptoms
4.1.2. Behavior
4.1.3. Medication
4.1.4. Environmental variables
4.2. Online Mood Tracking
4.2.1. healthyplace.com mood journal
4.2.2. moodchart.org
4.2.2.1. part of a research study
4.2.2.2. Sends daily email summaries.
4.2.2.3. Allows easy restrospective charting.
4.3. Offline Mood Charts
4.3.1. Software
4.3.1.1. bStable
4.3.1.1.1. Comprehensive system for
4.3.1.1.2. Tracks:
4.3.1.1.3. from McGraw Systems for $99
4.3.2. Printable
4.3.2.1. Monthly charts
4.3.2.1.1. Excel or PDF
4.3.2.1.2. Succinct introduction to charting
4.3.2.2. Charts for children
4.3.2.2.1. Very accessible for kids!
4.3.2.3. Blank chart and example
4.3.2.4. Mass General Mood Chart (PDF)
4.3.2.5. NIMH Mood Chart (PDF)
5. Treatment
5.1. First Line: Pharmacotherapy
5.1.1. MONITOR CLOSELY!
5.1.1.1. Encourage parents to monitor and chart symptoms and side effects
5.1.1.2. Don't let side effects settle in too long.
5.1.1.3. Small changes in meds can sometimes make a big difference.
5.1.2. Encourage use of Pharmacotherapy Algorithm
5.1.2.1. Algorithm Diagram (PDF)
5.1.2.2. Link to more info
5.1.3. Know principles of EOBPD prescription hygiene
5.1.3.1. Obtain history
5.1.3.2. Rapidly wean off all ineffective medications
5.1.3.3. Discontinue SSRIs
5.1.3.4. Discontinue stimulants
5.1.4. Work closely with pediatricians/MHMR doctors/psychiatrists
5.1.5. Let parents know it can sometimes take a long time to get the meds adjusted correctly
5.1.6. Know the meds
5.1.6.1. Traditional mood stabilzers
5.1.6.1.1. Lithium
5.1.6.1.2. Divalproex sodium (Depakote)
5.1.6.1.3. Carbamazepine (Tegretol)
5.1.6.1.4. Lamotrogine (Lamictal)
5.1.6.2. Atypical antipsychotics
5.1.6.2.1. Quetaipine (Seroquel)
5.1.6.2.2. Olanzapine (Zyprexa)
5.1.6.2.3. Ziprasidone (Geodon)
5.1.6.2.4. Risperidone (Risperdel)
5.2. Second Line: Psychsocial
5.2.1. CBT Intervention
5.2.1.1. Psychoeducation
5.2.1.2. Medication compliance
5.2.1.3. Mood monitoring
5.2.1.4. Modify unhelpful thinking
5.2.1.5. Identify stressors/triggers
5.2.1.6. Family Communication
5.2.1.7. Sleep maintenance
5.2.2. Child- and Family-Focused CBT
5.2.2.1. Grounded in biological theory of excessive reactivity
5.2.2.2. Description Document (Word doc)
5.2.2.3. Family conflict has high impact on symptoms
5.2.2.4. High levels of expressed emotion has negative impact too
5.2.3. Multi-family Psychoeducation Groups (MFPG)
5.2.4. Dialectical Behavior Therapy (DBT)
5.2.5. Interpersonal and Social Rhythm Therapy
5.3. Strategy for comorbid conditions
5.3.1. monitor and assess w/condition-specific instruments
5.3.2. Stabilize BPD symptoms
5.3.3. IF comorbid conditions have negative effect on functioning sequentially treat with
5.3.3.1. symptom specific medication
5.3.3.1.1. may aggravate BPD symptoms
5.3.3.2. psychosocial interventions
5.3.3.2.1. dont' generally cause mood dysregulation
5.4. Important Points
5.4.1. Family involvement CRUCIAL!!
5.4.2. Prescription hygiene critical.
5.4.3. Attack it from all sides.
5.4.3.1. medication
5.4.3.2. parent education
5.4.3.3. psychosocial therapy
5.4.3.4. web-based support
5.4.4. Assess for suicide.
6. EOPBD Controversies
6.1. Does it exist?
6.1.1. Three lines of evidence
6.1.1.1. One of the most heritable of the mental illnesses.
6.1.1.2. Adult form more common and earlier age of onset than previously recognized.
6.1.1.3. Efforts to validate the construct warrants additional investigation.
6.2. Is it over-diagnosed?
6.2.1. Possible reasons for "popularity" of diagnosis
6.2.1.1. Scholarly/medical research increased
6.2.1.2. BPParents ListServ
6.2.1.3. Papalos and Papalos 1999 book The Bipolar Child
6.2.1.4. Increased media exposure
6.2.1.5. Pharmaceutical advertising
6.2.1.6. Pharmaceutical company provided mood charting
6.3. Disagreement in the profession
6.3.1. Inconsistent diagnostic criteria
6.3.2. Inconsistent research design
6.3.3. Inconsistent terminology
6.3.4. Inconsistencies considered by some to be a black mark on the entire profession
7. Resources
7.1. Online Resources
7.1.1. NIMH-Bipolar Disorder in Children
7.1.2. www.depressedteens.com
7.1.3. Childhood and Adolescent Bipolar Foundation
7.1.3.1. About Bipolar Disorder in Children
7.1.3.2. Bookstore
7.1.3.3. Resource Links
7.1.3.4. research articles
7.1.4. Depression and Bipolar Support Alliance
7.1.5. American Academy of Childhood and Adolescent Psychiatry (AACAP) Bipolar Info
7.1.5.1. Excellent resource page
7.1.5.2. Facts for Families page
7.1.6. Facing Us
7.1.6.1. Depression and Bipolar Support Alliance site
7.1.6.2. An online "clubhouse"
7.1.6.3. "peer-based, recovery-oriented empowering services and resources when, where and how they want them."
7.1.7. Georgia Childhood Bipolar Foundation
7.1.7.1. Techniques for dealing with a Bipolar Child
7.1.8. Juvenile Bipolar Support Alliance
7.2. Books
7.2.1. List of Books for Children
7.2.2. Interactive Book for Young Children
7.2.3. List of Books for Parents
7.2.4. The Life of a Bipolar Child: What Every Parent and Professional Needs to Know. 2000. T. Carlson
7.2.5. Understanding and Educating Children and Adolescents with Bipolar Disorder: A Guide for Educators. 2003. M. Andersen, J.
7.3. Videos
7.3.1. Rescuing Childhood: Understanding Bipolar Disorder in Children and Adolescents
7.3.2. News Story
7.3.3. Bipolar Disorder: A Documentary
7.3.4. Good Growing: Bipolar Disorder
7.3.5. List of DVDs/Audio
