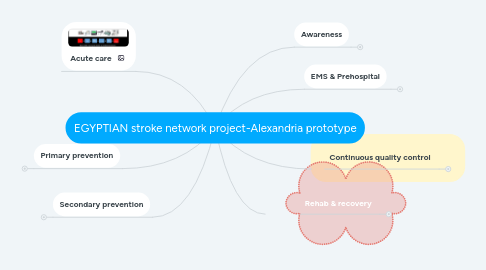
1. Secondary prevention
1.1. 1-Working with other specialities protocol (WOS-PROTOCOL) , cardiologists , radiologists, hematologist , vascular medicine, rheumatologist , pediatric neurologists , neurosurgeon, vascular surgery
1.2. Primary health units either direct or via medical convoys
1.3. Social media campaigns
1.4. House officer training program to be settled down during their stay
1.5. Training & educating non neurologists health dealers
2. Primary prevention
2.1. As above plus targeting
2.2. Primary health units either direct or via medical convoys
2.3. House officer training program to be settled down during their stay
2.4. Training & educating non neurologists health dealers
3. Acute care
4. Awareness
4.1. Brochures in medical points of care
4.2. Social media campaigns
4.3. External banners
4.4. Branding ambulance cares , public transportation , etc
4.5. Coordinating with national charity organization
5. EMS & Prehospital
5.1. ER Education & training with protocols assignment
5.1.1. ER ACTION PLAN MODELS TO BE IMPLEMENTED
5.2. Notify Pick-up recognize dispatch/delivery WEB (NPRD-WEB)
5.2.1. NPRD-WEB INFRASTRUCTURE
5.2.1.1. Notifications hotlines : 1. Landline fixed number 080000009095 1. Stroke@Ehotline ; 61212.tel 1. Sectorizing alexandria districts 6 districts 1. Registering ambulance cars and drivers
5.2.1.2. Stroke application with GPS capabilities to guide pick-up , recognization , dispatching/delivery
5.3. Hospital registration
5.3.1. Hospital agreement consensus
5.3.2. Hospital transparency unified policy
5.3.3. Classification system to catogroize the level of stroke services presented
5.3.3.1. I Neuroimaging availability II ICU services III Laboratory services IV No. of Beds or bed/services ratio V Neurosurgery availability VI Neurointervention availability VII cardiologist availability VIII vascular surgeon availability IX center connectivity and role in network X registry and clinical research XI reporting and transparency XII rehab and prevention accessibility
5.3.3.1.1. Level 3
5.3.3.1.2. Level 2
5.3.3.1.3. Level 1
5.3.4. Meterics preparation & implementations
5.3.4.1. documentation of presenting NIHSS
5.3.4.2. docu- mentation of the 90-day mRS outcome,
5.3.4.3. documentation of the overall rate of hemorrhagic transformation of an AIS
5.3.4.4. the median time to revascularization, and CSTK
5.3.4.4.1. – First medical contact to hospital arrival – Time from hospital arrival to stroke team evaluation – Time from hospital arrival to imaging (if necessary) • Recommended less than 10 min
5.3.4.4.2. – Time from imaging study to groin puncture • Recommended less than 60 min – Time from hospital arrival to groin puncture • Recommended less than 90 min – Time from groin puncture to first MT attempt • Recommended less than 30 min – Time from groin puncture to TICI 2B or better or conclusion of procedure • Recommended less than 60 min
5.3.4.4.3. Other critical procedural data include the following: – Preoperative ASPECTs score and core infarct volume (on baseline CT or MR) – Location of LVO on preoperative vascular imaging and initial diagnostic cerebral angiogram – Preintervention TICI score – Use of procedural general anesthesia versus conscious sedation – Postintervention infarct volume – Endovascular complications • Intracranial vessel perforation • Embolization to previously uninvolved territory • Arterial dissection • Groin hematoma requiring transfusion or surgical repair
5.3.4.4.4. clinical outcome measures – NIHSS at 24 h and hospital discharge – Symptomatic intracranial hemorrhage – Discharge destination – mRS and NIHSS at discharge and 90 days – Hospital and 90-day mortality
5.3.4.4.5. the postintervention TICI reperfusion score
