1. Pathophysiology
1.1. Airflow is obstructed throughout the lungs due to chronic inflammation of the tissue.
2. Risk factors
2.1. Tobacco smoking, gas exposure, air pollution, alpha-1-antitrypsin deficiency.
3. Patient history
3.1. 71 year old female seen in the Emergency Department for an exacerbation of COPD. Symptoms: increased shortness of breath, productive cough with white to clear sputum, activity intolerance. She uses 2L of O2 at home when needed.
4. Vital signs
4.1. Heart rate: 88 Respiratory rate: 28 Oxygen saturation: 82% on room air Blood pressure: 132/82 Temperature: 98.8F
5. Allergies
5.1. No known allergies.
6. Home medications
6.1. 2L of oxygen by nasal cannula PRN. DuoNeb inhalation solution: 3 mL vial by nebulization 4 times a day. Albuterol inhalation solution: 2 puffs every 4 hours PRN. 81 mg chewable aspirin. 60 mcg tablet levothyroxine daily.
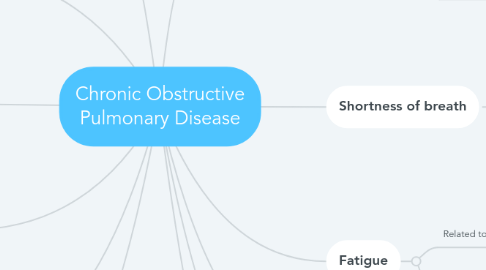
7. Shortness of breath
7.1. Related to impaired gas exchange
7.1.1. Goal: patient maintains optimal gas exchange
7.1.1.1. Interventions: apply oxygen by nasal cannula as needed; allow for rest breaks during activity
7.2. Related to impaired physical mobility
7.2.1. Goal: patient performs activities independently
7.2.1.1. Interventions: provide a safe environment
7.3. Related to impaired spontaneous ventilation
7.3.1. Goal: patient maintains regular and unlabored breathing pattern
7.3.1.1. Interventions: keep HOB elevated to at least 45 degrees; use oxygen by cannula as needed
8. Fatigue
8.1. Related to activity intolerance
8.1.1. Goal: patient will use energy conserving techniques
8.1.1.1. Interventions: evaluate need for extra help at home; encourage the patient to move slowly
8.2. Related to self-care deficit
8.2.1. Goal: patient will identify relevant resources to complete activities of daily living
8.2.1.1. Interventions: establish short-term goals; provide positive-reinforcement
9. Chronic productive cough
9.1. Related to impaired swallowing
9.1.1. Goal: patient will demonstrate ability to swallow safely
9.1.1.1. Interventions: consult a speech pathologist; provide oral care before and after meals
9.2. Related to ineffective airway clearance
9.2.1. Goal: patient will maintain clear lung sounds in all lobes
9.2.1.1. Interventions: promote cough and deep breathing
9.3. Related to readiness for enhanced comfort
9.3.1. Goal: patient will verbalize feelings of comfort
9.3.1.1. Interventions: manage pain; suction airway as needed
10. Tests/labs
10.1. Chest x-ray showed no abnormalities.
10.1.1. CBC results were within normal limits, except the neutrophils (elevated: 9,000/mm3).
10.1.1.1. Sputum culture showed presence of Haemophilus influenzae.
11. Plan of care
11.1. Administer cefixime IV 400 mg and fluid bolus of 1,000 mL of 0.9% normal saline wide open.
11.1.1. Administer 4L of humidified O2 by nasal cannula for desired oxygen saturation of 90% or above.
11.1.1.1. Discharge after medication administration with referral to primary care physician in the next 1-3 days.
12. Comorbidity of COPD
12.1. Gastroesophageal reflux (GERD)
12.1.1. This patient developed GERD 1 year after she was diagnosed with COPD.
12.1.1.1. GERD occurs due to the frequent coughing and shortness of breath in a COPD patient. This causes the valve at the top of the stomach to open up, allowing acids to go up the esophagus. This can also cause more frequent flare ups of COPD due to the irritation in the trachea/lungs.
12.1.1.1.1. Treatment: the patient should avoid triggering foods, such as spicy foods and alcoholic drinks. The patient should sleep with the head of their bed elevated or with multiple pillows. There are over-the-counter as well as prescription medications the patient can take to control GERD symptoms.

