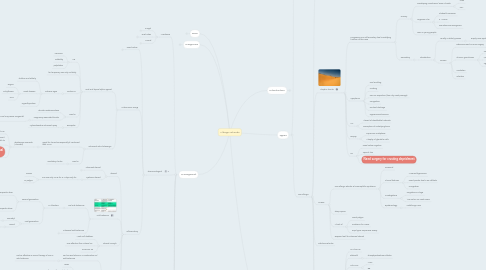
1. Managment
1.1. Avoidance
1.1.1. Fungal
1.1.1.1. Remove of moistures surfaces
1.1.1.2. Replacement of contaminated material
1.1.1.3. diluted bleach on non-porus surface
1.1.1.3.1. e.g. glasses
1.1.1.3.2. With fungocide
1.1.1.4. Keep humudity <50%
1.1.1.5. HEPPA filter
1.1.2. Dust mites
1.1.2.1. Control humidity to <50%
1.1.2.2. Dust mite cover for beddings
1.1.2.3. Use HEPA
1.1.2.3.1. High efficiency Particulate Air
1.1.2.4. Vaccum Carpenting
1.1.2.5. Use of acaricides
1.1.2.6. Wash bedding in hot water
1.1.3. Animal
1.1.3.1. May take >6months of allergen to go away
1.1.3.2. HEPPA filter
1.1.3.3. Ask someone to wash to the animal with warm water once a week
1.1.3.4. Keep them out side of the bedroom
1.2. Pharmacological
1.2.1. Nasal Saline
1.2.1.1. effective
1.2.2. Automnomic Drugs
1.2.2.1. Oral and topical alpha agonist
1.2.2.1.1. S.E
1.2.2.1.2. for temporary use only not daily
1.2.2.1.3. Caution in
1.2.2.1.4. Used in
1.2.2.1.5. Examples
1.2.2.2. Intranasal anti-cholenergic
1.2.2.2.1. good for rhinorrhea especially if combined with IN CS
1.2.2.2.2. Used in
1.2.3. Inflammatory
1.2.3.1. Steroid
1.2.3.1.1. Intranasal steroid
1.2.3.1.2. Systemic steroid
1.2.3.2. Anti-histamine
1.2.3.2.1. oral anti-histamine
1.2.3.2.2. Intranasal anti-histamine
1.2.3.3. Intrasal cromyln
1.2.3.3.1. Mast Cell stabilizer
1.2.3.3.2. Less effective than Intrasal CS
1.2.3.3.3. minimum SE
1.2.3.4. Oral anti-LT
1.2.3.4.1. can be used alone or in combination w/ anti-histamine
1.2.3.4.2. Particularly effective
1.2.3.4.3. The only approved is Montelukast
1.2.3.5. Omalizumab
1.2.3.5.1. effective but not approved yet
1.3. Immunotherapy
1.3.1. Indications
1.3.1.1. Evidence of sensitization to clinically relavent aeroallergen
1.3.1.2. Failed, intolerance or not preferred pharmacological Rx.
1.3.2. Advantages
1.3.2.1. can prevent the sensitization of other allergen
1.3.2.2. Prevent the development of asthma
1.4. Surgery
1.4.1. for comorbidities
1.4.1.1. Septal deviation
1.4.1.2. Inferior turbinate hyper trophy
1.4.1.3. sinusitis complication
1.4.1.4. adenoid hypertrophy
1.5. Special Consideration
1.5.1. Pregnancy
1.5.1.1. Check safety of meds
1.5.1.1.1. Avoid oral decongestant in the 1st trimester
1.5.1.1.2. Anti-histamines,IN CS, cromyln, montelukast are safe
1.5.1.2. No initiation or escalation of IT
2. Diagnosis
2.1. SPT and sIgE
2.1.1. 70-75%sensitivity
2.1.1.1. for which 1/4 pt will have -ve testing yet have true allergic disease despite it is the best test.
2.1.1.1.1. For which you may one offer Rx. despite negative allergy testing
2.2. Elevated IgE and Eo
2.2.1. Have limited utility
2.2.1.1. Typically
2.2.1.1.1. IgE>140IU/ml
2.2.1.1.2. Eo > 80cells/ml
2.2.1.2. Very variable
2.2.1.2.1. Not used in Dx
2.3. Nasal Nitric Oxide
2.3.1. Increase in Allergic Rhinitis
2.3.2. Decrease in sinus infection
2.4. Medication to avoid prior to SPT because they suppress
2.4.1. all anti-histamine
2.4.1.1. Including Azelastine
2.4.1.1.1. Intra-nasal anti-histamine
2.4.2. Steroid >20mg
2.4.3. Tacrolimus interfer
2.4.3.1. It is OK to use
2.4.3.1.1. Pimecrolimus
2.4.3.1.2. CSA
2.4.4. Omalizumab after 6 months
2.4.5. Psychiatric medications
2.4.5.1. TCA
2.4.5.2. Benzodiazepine
2.4.5.3. Quitiapine
2.4.5.3.1. Anti-psychotic
3. DDx
3.1. Pre-school age
3.1.1. Foreign body
3.1.2. CSF leak
3.1.2.1. Hx of trauma
3.1.2.2. Colorless
3.1.3. CF/PCD/Immunodeficiency
3.1.4. Coanal atresia
3.1.5. Deviated Septum
3.1.6. Adenoidal Hypertrophy
3.1.7. Coaguloapthy
4. Introduction
4.1. Allergen
4.1.1. Airborn
4.1.1.1. Protein or glycprotein
4.1.1.2. activity
4.1.1.2.1. Some have protease activity
4.1.1.2.2. Activate epithelial cells
4.1.2. Hapten
4.1.2.1. Drugs
4.1.2.2. Occupational agent
4.2. Inflammatory mediattors
4.2.1. Immediate
4.2.1.1. Preformed mediators
4.2.1.1.1. Histamines
4.2.1.1.2. Heparin
4.2.1.1.3. Proteases
4.2.1.1.4. Kinins
4.2.1.1.5. Another way to remember it 2H 2C 2T
4.2.1.2. Newly formed
4.2.1.2.1. Prostaglandins
4.2.1.2.2. Leukotriens
4.2.1.2.3. Thromboxoane
4.2.2. Late phase
4.2.2.1. Congestion!
4.2.2.2. Begin 4-8hrs and last >24hrs
4.2.2.3. cells
4.2.2.3.1. Basophills
4.2.2.3.2. Eosinophils
4.2.2.3.3. Th2
5. Types
5.1. Allergic
5.1.1. Types
5.1.1.1. Seasonal vs. Perinnial
5.1.1.1.1. Perennial with seasonal exacerbation
5.1.1.1.2. Seasonal 20%
5.1.1.1.3. Perennial 40%
5.1.1.1.4. Episodic
5.1.1.2. Severity and duration
5.1.1.2.1. ARIA Classification
5.1.2. Epidemiology
5.1.2.1. Prevalence 20%
5.1.2.2. 80% onset <age 20 yo
5.2. Non-allergic
5.2.1. Vasomotor (idiopathic)
5.2.1.1. 3 criteria
5.2.1.1.1. Not infectious
5.2.1.1.2. Not allergic
5.2.1.1.3. No eosinophillia
5.2.1.2. Heterogenous group
5.2.1.2.1. autonomic dysfunction
5.2.1.3. Triggers
5.2.1.3.1. Cold air
5.2.1.3.2. Dry air
5.2.1.3.3. Barometric pressure
5.2.1.3.4. Strong scent
5.2.1.3.5. IF trigger by food-->vagal Gustatory Rhinitis (specific food: capsaicin)
5.2.1.3.6. Athlete rhinitis
5.2.1.4. Rhinorrhea prominent symptoms
5.2.1.4.1. Rx intranasal anti-histamine
5.2.2. Atrophic rhinitis
5.2.2.1. Progressive non-inflammatory loss humidifying function of the nose
5.2.2.1.1. Primary
5.2.2.1.2. Secondary
5.2.2.2. Symptoms
5.2.2.2.1. Foul smelling
5.2.2.2.2. Crusting
5.2.2.2.3. Pain on inspiration (from dry nasal passage)
5.2.2.2.4. Congestion
5.2.2.2.5. Purulant dischage
5.2.2.2.6. Hyposomnia/anosmia
5.2.2.3. CT:
5.2.2.3.1. Absent of identifiable turbinate
5.2.2.3.2. Resorption of underlying bone
5.2.2.4. Biopsy
5.2.2.4.1. Squamous metaplasia
5.2.2.4.2. Atrophy of glandular cells
5.2.2.5. Rx
5.2.2.5.1. Nasal saline irrigation
5.2.2.5.2. Topical Abx
5.2.2.5.3. Need surgery for crusting depridment
5.2.3. NARES
5.2.3.1. Non-allergic Rhinitis w/ eosinophillia Syndrome
5.2.3.1.1. Perennial
5.2.3.1.2. Clinical features
5.2.3.1.3. Investigations
5.2.3.1.4. Epidemiology
5.2.3.2. Sleep apnea
5.2.3.3. At risk of
5.2.3.3.1. Nasal polyps
5.2.3.3.2. Predrome for AERD
5.2.3.3.3. 50% hyper responsive airway
5.2.3.4. Respond well to intranasal steroid
5.2.4. Infectious Rhinitis
5.2.5. Medication induce rhintiis
5.2.5.1. ASA/NSAID
5.2.5.2. Sildenafil
5.2.5.2.1. Phosphpodiestrase inhbitor
5.2.5.3. Anti-HTN
5.2.5.3.1. ACEI
5.2.5.3.2. BB
5.2.5.4. Rhinitis medicametnosa
5.2.5.4.1. To treat it, use
5.2.5.5. OCP
5.2.5.6. Illicit drugs
5.2.5.6.1. coccaine
5.2.5.6.2. Metamphetamine
5.2.6. Hormon-induce rhinitis
5.2.6.1. OCP
5.2.6.2. Puberty
5.2.6.3. Pregnancy
5.2.6.3.1. The most common is AR that gets worse in 1/3 of pregnant women
5.2.6.3.2. Pregnancy assosciated
5.2.6.4. Hypotherodism
