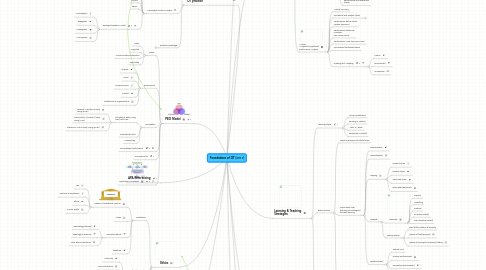
1. 3 types of knowledge to support OT practice
1.1. Paradigms
1.1.1. New Emerging Paradigm (1980s-today)
1.1.2. Crisis (1970s)
1.1.3. Mechanistic Paradigm (1960s)
1.1.4. Crisis (1950s)
1.1.5. Paradigm of Occupation (1900-1940s)
1.1.6. Moral Treatment (18th-19th centuries)
1.2. Conceptual Practice Models
1.2.1. PEO
1.2.2. CMOP-E
1.2.3. Kawa
1.2.4. MOHO
1.2.5. PEOP
1.2.6. Ecological Systems Model
1.2.6.1. Macrosystem
1.2.6.2. Exosystem
1.2.6.3. Mesosystem
1.2.6.4. Microsystem
1.3. Related Knowledge
1.3.1. Anatomy
1.3.2. Psychology
1.3.3. Neuroscience
1.3.4. Social Work
1.3.5. General Medicine
2. PEO Model
2.1. Person
2.1.1. Motor
2.1.2. Cognitive
2.1.3. Communication/Interaction
2.1.4. Spirituality
2.2. Environment
2.2.1. Physical
2.2.2. Social
2.2.3. Socioeconomic
2.2.4. Cultural
2.2.5. Institutional & Organisational
2.3. Occupation
2.3.1. Activities of Daily Living (ADL)/Self Care
2.3.1.1. Personal Activities of Daily Living (PADL)
2.3.1.2. Instrumental Activities of Daily Living (IADL)
2.3.1.3. Electronic Aids to Daily Living (EADL)
2.3.2. Productivity/Work
2.3.3. Leisure/Play
2.4. Occupational Performance
2.5. Occupationl fit
2.6. Application Framework
3. APA Referencing
4. Clinical Reasoning
4.1. Scientific Reasoning
4.1.1. Diagnostic
4.1.2. Procedural
4.2. Narrative Reasoning
4.3. Pragmatic Reasoning
4.4. Ethical Reasoning
4.5. Interactive Reasoning
5. Ethics
5.1. Definitions
5.1.1. House of Professional Practice
5.1.1.1. Law
5.1.1.2. Technical Competence
5.1.1.3. Ethics
5.1.1.4. Human Rights
5.1.2. Values
5.1.3. Normative Ethics
5.1.3.1. Deontology (decree)
5.1.3.2. Teleology (outcomes)
5.1.3.3. Virtue Ethics (intentions)
5.1.4. Bioethics
5.2. Bioethical Principles
5.2.1. Autonomy
5.2.2. Non-maleficence
5.2.3. Beneficence
5.2.4. Justice
5.3. Bioethical rules
5.3.1. Veracity
5.3.2. Confidentiality
5.4. Ethical Grid
6. Client-centered Practice
6.1. Person-centered
6.2. Client-centered
6.3. Therapeutic relationship
6.3.1. Develop rapport
6.3.2. Establish trust
6.3.3. Develop a collaborative partnership
6.3.4. Sustain the therapeutic relationship
6.3.5. Enduring relationship
6.4. Best practices
6.5. Barriers
7. Canadian Practice Process Framework (CPPF)
7.1. Enter/initiate
7.2. Set the stage
7.3. Assess/evaluate
7.4. Agree on objectives
7.5. Implement/plan
7.6. Monitor/modify
7.7. Evaluate outcomes
7.8. Conclude/exit
8. Reflective Practice
8.1. Kolb's Learning Cycle
8.1.1. Active Experimentation
8.1.2. Concrete Experience
8.1.3. Reflective Observation
8.1.4. Abstract Conceptualisation
8.2. Strands of Reflection
8.2.1. Factual Strand
8.2.2. Retrospective Strand
8.2.3. Sub-stratum Strand
8.2.4. Connective Strand
9. Learning & Teaching Strategies
9.1. Learning Styles
9.1.1. Active vs Reflective
9.1.2. Sensing vs Intuitive
9.1.3. Visual vs Verbal
9.1.4. Sequential vs Global
9.2. Best practices
9.2.1. Teach in presence of natural cues
9.2.2. Instructional aids (behavioural strategies) to assist learning
9.2.2.1. Discrimination
9.2.2.2. Generalisation
9.2.2.3. Shaping
9.2.2.3.1. Forward Chain
9.2.2.3.2. Reverse Chain
9.2.2.3.3. Total Task Chain
9.2.2.3.4. Interrupted behaviour
9.2.2.4. Prompts
9.2.2.4.1. Hierarchy
9.2.2.4.2. Best practices
9.2.2.5. Reinforcement
9.2.2.5.1. Natural cues
9.2.2.5.2. Primary reinforcement
9.2.2.5.3. Secondary reinforcement
9.2.2.5.4. Positive/Negative reinforcement
9.2.3. Provide feedback
9.3. Errorless learning
10. Assessments
10.1. Semi-structured interview
10.1.1. SOLER
10.1.1.1. Squarely face
10.1.1.2. Open posture
10.1.1.3. Lean slightly
10.1.1.4. Eye contact
10.1.1.5. Relaxed posture (non-verbal)
10.1.2. Active listening
10.1.2.1. Joining by preparing
10.1.2.2. Joining by attending
10.1.2.3. Following skills
10.1.2.4. Reflecting skills
10.1.2.5. Drawing to a conclusion
10.1.3. Open-ended questions
10.2. Occupational Story
10.2.1. Narrative process
10.2.1.1. Restitution narrative
10.2.1.2. Chaos narrative
10.2.1.3. Quest narrative
10.3. Canadian Occupational Performance Measure (COPM)
10.3.1. Step 1: Identifying occupational performance issues (semi-structured interview)
10.3.1.1. Self-care
10.3.1.1.1. Personal care
10.3.1.1.2. Functional mobility
10.3.1.1.3. Community management
10.3.1.2. Productivity
10.3.1.2.1. Paid/unpaid work
10.3.1.2.2. Household management
10.3.1.2.3. School
10.3.1.2.4. Play
10.3.1.3. Leisure
10.3.1.3.1. Quiet recreation
10.3.1.3.2. Active recreation
10.3.1.3.3. Socialisation
10.3.2. Step 2: Rate importance for each issue
10.3.3. Step 3: Choose most important items
10.3.4. Step 4: Rate performance and satisfaction
10.3.5. Step 5: Calculate total performance and satisfaction scores
10.4. Activity Analysis/Occupational Performance Analysis
10.4.1. Activity summary
10.4.2. Procedural task analysis (Yuen)
10.4.2.1. Identify task
10.4.2.2. Identify criterion for completion of task
10.4.2.3. Construct the contents & steps
10.4.2.4. Validate contents & steps
10.4.2.5. Tailor for individual needs
10.4.3. Performance skills & Client Factors (PERSON)
10.4.4. Performance Patterns & Contexts (ENVIRONMENT)
10.4.5. Performance Areas (OCCUPATION)
10.4.6. Precautions/Contraindications
10.4.7. Grading and Adapting
10.4.7.1. Person
10.4.7.2. Environment
10.4.7.3. Occupation
11. Evidence-based Practice
11.1. Practice cycle
11.1.1. Identify problem (clinical question)
11.1.2. Gather evidence
11.1.3. Appraise/evaluate evidence
11.1.4. Communicate evidence
11.1.5. Implement and Review
11.2. Good sources of evidence
11.2.1. McMaster University (School of Rehabilitation Science)
11.2.2. OT Seeker
11.2.3. Cochrane Collaboration
11.3. Types
11.3.1. Research & Clinical Expertise
11.3.1.1. Levels
11.3.1.1.1. Level 1:Randomised controlled trials
11.3.1.1.2. Level II-1: Non-randomised trials
11.3.1.1.3. Level II-2: Non-randomised trials (with historical or location controls)
11.3.1.1.4. Level II-3: Case series without controls
11.3.1.1.5. Level III: Opinions (authorities, studies, expert committees)
11.3.1.2. Categories
11.3.1.2.1. Descriptive
11.3.1.2.2. Assessment
11.3.1.2.3. Effectiveness
11.3.1.2.4. Responsiveness
11.3.2. Clients' beliefs & values
11.3.3. Clients' clinical assessments
11.3.4. Clients' preferences
