1. Post-Op Checklist First Hour Expect labs/correction in OR as well.
1.1. Ventilator: PCV: PI: 18-22; Peep 8-10; FIO2 goal 21% (Max 30-40%) I/E : 1/2 * Change in FIO2 requirements call Transplant
1.2. POC: iStat Electrolytes, INR, H/H, ROTEM
1.3. Keep Hb > 9-10:Refer to transfusion algorithm
1.3.1. Correct coagulopathies + platelet count in 1 hour. Goals PLT> 80; INR <1.6; Fibrinogen>200; If bleeding by our criterion or elevated PTT, check ACT.
1.3.2. CBC, CHEM, INR, PTT, PT, Fibrinogen, Lactic acid, electrolytes q 3-4 hours
1.3.3. CHEST TUBE OUTPUT> 200ml/HR or If > 100ml for 3 hrs, please call Transplant Surgery
1.4. Albumin for volume resuscitation
1.5. STAT ABG: Assistance from respiratory for low tidal volume strategy
1.5.1. Monitors in place and all functioning with arrival (goal within15 minutes)
1.6. CERNER Documentation: Vitals, SVO2, I+O q 15 minutes for first 2 hours then q 30 minutes for the next 2 hours. After any titration of drips, needs closer documentation of parameters (q15 minutes) until stable.
1.7. Stat CXR ( pleural hematoma; Check CT tubes positioning; PGD)
1.8. Sedation- Goal Patient awake and comfortable. Use Precedex, Ketamine. (Judicious Propofol and pain medications).
1.8.1. Hourly charting of SVO2, Chest Tube, and Urine Output ( Cerner)
1.9. Preferred INOTROPES- Epinephrine, Milrinone, Dopamine. Vasopressin as needed. (Judicious Levaphed due to theoretic ischemia to surgical anastomosis)
1.10. Temperature> 101 panculture immediately as Lung transplant donors/recipients colonized with organisms.
2. Respiratory
2.1. Ventilator: PCV; PI: 18-22; Peep 8-10; FIO2 goal 21% (Max 30-40%) ; I/E : 1/2 * Call if change in FIO2 requirements call Transplant
2.2. CXR DAILY
2.3. ABG q 4 hr
2.4. iNO: 20 ppm
2.4.1. Chest PT, Mucolytics, Hypertonic saline q4-6 hours
2.5. CT tube output >200ml/hr call TX/ICU of >100ml/hr for 3 hrs. please call Transplant Surgery.
2.5.1. CT tube with new air leak please notify: Surgery/Tx and keep on suction ( must be transported on suction)
2.6. Contact Tx/ICU for change in FIO2, PH< 7.2, or drop in tidal volume on PCV
2.6.1. ECMO?: Escalating FIO2 , change in CXR or compliance of lung.
2.6.2. Obtain repeat CXR STAT: Hematoma, Infiltrates, Pneumothorax
2.6.3. Consider recruitment maneuver for atelectasis
2.6.4. Bronchoscopy: Rule out Torsion ( crescent sign), mucus plugs, PNA, Bronchorrhea-Pulmonary EDEMA, ischemic reperfusion injury, * Note Laterality and Segmental Changes.
2.7. Ventilatory WEANING
2.7.1. REMOVE DIAPHRAGM STITCHES
2.7.2. Goal is early extubation if possible. DO NOT EXTUBATE without performing BRONCHSCOPY first
2.7.3. RSBI on 5/5 and NIFF <-20
2.7.3.1. LOW BP: Vasopressin preferred. Judicious levaphed due to airways ischemia. Low BP and low output, requires Volume and increase inotropic agents
2.7.4. BRONCHOSCOPY FREQUENTLY: Rule out Torsion, dehiscence, mucus plugs, PNA, bronchorrhea-pulm edema, ischemia reperfusion injury. * Minimize use of lavage fluid as organ has no lymphatic drainage.
2.7.5. Parameters: Mental status, FIO2 <30%, Stable hemodynamics, improving lactic acid, diuresis occurring, CXR no pleural problems or bleeding, adequate pain control.
2.7.6. FAILED Extubation warrants early trach discussion due to early physical mobilization in lung transplantation.
2.7.7. Trach collar trials to continue as long as PH is not less than 7.25; No indication for T piece.
3. Neurologic/Pain
3.1. GOAL: ALERT AWAKE, FOLLOWING COMMANDS, walking if able ( not heavily sedated).
3.2. Avoid respiratory depressants. Favor precedex and ketamine... Propofol and low benzodiazepines must be used sparingly due to complications
3.3. PAIN CONTROL: Dilaudid 0.2- 0.5 mg IV q 4-6 hours + OFIRMEV + ROBAXIN (IV to PO). GABAPENTIN for neuropathic pain
3.4. Minimal Narcotics: If high requirements consider epidural-nerve block or paravertebral block
3.5. Anxiety: Buspar,Olanzapine , Celexa, QTC monitoring required
4. Allograft: No Lymphatics
4.1. CXR Daily for PTX, Effusions, PGD, PNA, Lines/Tube placement
4.2. Bronchoscopy: Torsion, mucus plugs, PNA, PGD, bronchorrhea.
4.3. IMMUNOSUPPRESSION
4.3.1. Cellcept/Imuran
4.3.2. Steroids
4.3.2.1. PROGRAF/TACROLIMUS is SUBLINGUAL ( capsule opened first and powder under the tongue) until transitioned to ORAL Regimen. Check Prograf or cyclosporine level q am before AM dose
4.3.3. OTHER: Basiliximab ( POD #1 and #4); Belatacept; IVIG 0.5mg/kg
4.4. Prophylaxis
4.4.1. Fungus: Inhaled Abelcept; Voriconazole, Posaconazole, Cresemba
4.4.2. Bactrim, Mepron, Pentamidine > POD 7
4.4.3. CMV: Ganciclovir vs Valcyte: CMV PCR blood weekly after transplant
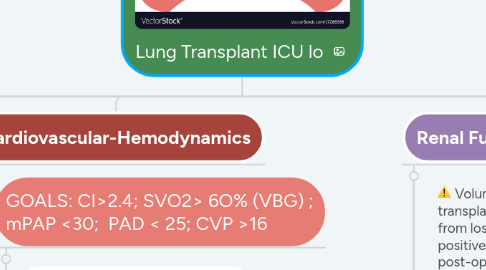
5. Cardiovascular-Hemodynamics
5.1. GOALS: CI>2.4; SVO2> 6O% (VBG) ; mPAP <30; PAD < 25; CVP >16
5.1.1. X
5.1.2. Stroke Volume: TEE or ECHO
5.1.2.1. Hemoglobin > 9
5.1.3. CONTACT TX-ICU for persistent low SVO2
5.1.4. CONTACT ICU and TRANSPLANT TEAM for large changes in requirements ( Ex 0.03->0.07). If with large inotropic needs (Ex EPI 0.1), consider STAT TEE or imaCor for rule out TAMPONADE and other urgent issues.
5.1.5. ATRIAL Fibrillation
5.1.5.1. UNSTABLE: DC cardioversion
5.1.5.2. STABLE: Amiodarone preference: 300 mg IV once--> 150 mg once-->150 once then start IV drip. If persistent after 3-6 hours consider DC cardioversion ( trying to avoid need to start anticoagulation)
5.2. HIGH BP>160/90: Titrate milrinone if running, can give IV Cardene or Clevidipine. Avoid IV nitrates as they cause shunt physiology in lung transplant recipients. Treat Anxiety and Pain if hyperdynamic. Understand relationship between BP and CI ( table above)
6. Renal Function-Volume
6.1. Volume removal needed for lung transplant due to capillary leak from loss of lymphatics and positive fluid balance post-operatively
6.2. Contact ICU for increase in Creatinine that is 1.5x baseline.
6.2.1. Call transplant for Anuria
6.3. Consider diuresis as lactic acid levels and hemodynamics improve
6.4. IV Lasix versus Lasix drip 5-10 mg /hr if urine output less than 0.5cc/kg/hr vital signs stable
6.4.1. THROMBOCYTOPENIA: Check Hitt Ab, Obtain peripheral smear, stop offending agents, check ADAMTS13, Consider TTP/HUS or DITMA that requires pheresis.
6.5. If no response to Lasix, may require CRRT
6.6. Contact ICU for drop in urine output (<0.5 cc/kg) or if with Lasix failure.
7. Hematologic Goals
7.1. Immediate post-op if not Bleeding: Goal: PLT>80; HB> 9; WBC> 3; INR< 1.6; Normal fibrinogen level >200; If PTT elevated and there is bleeding check ACT
7.1.1. Early dobhoff placement under fluoro post-extubation if NPO > 5 days
