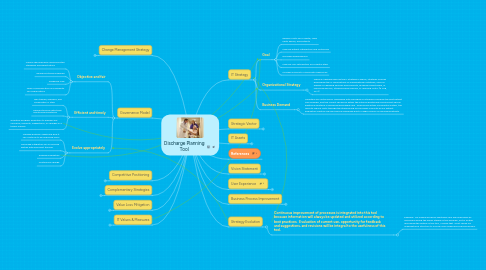
1. Change Management Strategy
1.1. Leadership
1.1.1. Team will need to create an impactful, easy to understand, outcome focused, presentation in order to communicate the need and usefulness of the program.
1.1.2. Leadership will need to continue to communicate, build trust, and participate in the change
1.1.3. Welcome feedback and suggestions from the staff in order to resolve issues and illustrate respect for the involved parties.
1.2. Language and Vision
1.2.1. Communicating effectively is pivotal when implementing change and gaining staff acceptance will be more likely if processes, objectives, and expectations are clearly and thoroughly understood. According to Weiss & Legrand, “A clearly defined framework greatly increases the probability of a successful outcome” (2011, p. 1616).
1.3. Connection and Trust
1.3.1. By making the program relatable and beneficial for all active parties, the staff will trust in the need for a change in process.
1.4. Incentives
1.5. Planning, Implementing, and Iterating
2. Governance Model
2.1. Objective and fair
2.1.1. Clearly specified and communicated standards and expectations
2.1.2. Desired outcomes defined
2.1.3. Feedback loop
2.1.4. Open communication and flexibility for modifications
2.2. Efficient and timely
2.2.1. Well trained, available, and cooperative IT staff
2.2.2. Defined timeline with team monitoring milestones
2.2.3. Quarterly program evaluation to address any concerns, requests, suggestions, or changes in a timely manner
2.3. Evolve appropriately
2.3.1. Manage program usage and how it can continue to be improved upon
2.3.2. Thorough integration for all involved parties with sufficient training
2.3.3. Program Evaluation
2.3.4. Continuous change
3. Competitive Positioning
3.1. Meaningful Use
3.1.1. Various other discharge planning tools provide avenues toward assisting with discharge arrangements and aggregating patient resources, but this program allows for a platform involving all interested parties including patients, inpatient care providers, outpatient care providers, third party payers, and vendors.
3.1.1.1. Patients participate in their individual care plan.
3.1.1.2. All users are able to provide feedback and suggestions for best practices
3.1.1.3. Evaluation of program
3.1.1.3.1. Cost savings
3.1.1.3.2. Competitive programs
3.1.1.3.3. Patient Satisfaction
3.1.1.3.4. Third Party Payer Feedback
3.1.1.3.5. Employee Feedback
3.2. Collaboration
3.2.1. Competitive positioning does not have to be divided, rather the Discharge Planning tool can be used with other programs or tools within the EHR. According to Ben Hecht in the Harvard Business Review, organizations "are putting aside self-interests and collaborating to build a new civic infrastructure to advance their shared objectives" (2013).
3.2.1.1. Leverage resources by complementing, conserving, concentrating, accumulating, and recovering (Mintzberg, Ahlstrand, & Lampel, 2011).
3.3. Quality Improvement
3.3.1. Mintzberg, Ahlstrand, & Lampel describe innovation as "the doing of new things or the doing of things that are already being done in a new way" (1998, p. 1717). These activities are already being done but are being done so in an inefficient way, so positioning this tool as an improvement from current processes will be important versus the alternative of continuing processes as is.
4. Complementary Strategies
4.1. Broad Leverage
4.1.1. Engaging in thoughtful innovation and creating a planning tool that unites all parties with the common goal of a successful patient outcome is the purpose of the discharge planning tool.
4.1.1.1. Establish effective governance
4.1.1.2. Frequent evaluation of IT utilization
4.1.1.3. Patient and Employee Feedback
4.2. Initiative Specific Strategies
4.2.1. According to Glaser & Salzberg, the effects of health care reform on IT strategy is "the advent of new care models that emphasize care coordination and accountability across care settings" (2011, p. 3704). EHR revolutionizes data preservation and data sharing to improve communication, facilitate better continuity of care, and improve patient outcomes. This discharge planning tool will further perpetuate the ease of using the digital world by complementing the EHR records with more thorough and interactive options.
5. Value Loss Mitigation
5.1. Contributor: Value of the IT program needs to be established and communicated to all involved parties.
5.1.1. Mitigation: Creating a governing body that creates a thorough plan, has team leaders dispersed amongst all contributing parties, prepares a well trained IT team, and specifies objectives and expectations
5.2. Contributor: Financial investment associated with implementing a new program
5.2.1. Mitigation: Clear criteria and expectations must be established with concrete baseline data. Realistic short and long term financial goals must be established. Periodic comparisons and evaluations must be made to determine the true, long-term financial impact of the program and what adjustments must be made.
5.3. Contributor: Inefficient training and support for employee usage
5.3.1. Mitigation: An effective IT team hired and a thorough training of the program prior to implementation. Team Leader assigned for further training and troubleshooting. IT department accessible to further assistance.
5.4. Contributor: Lack of program usefulness due to incomplete and irrelevant data collection and organization for staff and patient use
5.4.1. Mitigation: A team of individuals will be updating and organizing patient resources, patient assistance programs, community programs, and all relevant information in order to provide useful and accessible data.
5.4.1.1. Prescription Assistance Program
5.4.1.2. Medicare Equipment Suppliers
5.4.1.3. Medicare Home Health Services
6. IT Values & Measures
6.1. "IT can provide an advantage if it is used to thoughtfully improve core processes, provide critical data, and support product or service differentiation" (Glaser & Salzberg, 2011, p. 2643).
6.1.1. Financial Advantage - Hospitals are seeking to improve quality measures while minimizing costs through evaluating specific indicators such as length of stay, readmission rates, and overall costs of hospitalization (Carek, et al., 2008)
6.1.1.1. Less Readmissions
6.1.1.2. Shorter Length of Stay
6.1.1.3. Vendor Contracting
6.1.1.4. Third Party Reimbursement Rates
6.1.2. Patient Experience
6.1.2.1. Improved discharge plan
6.1.2.2. Utilization of resources
6.1.2.3. Patient program usage in developing treatment plan
6.1.2.4. Patient Admission Data
6.1.3. Employee Satisfaction
6.1.3.1. Improve processes
6.1.3.2. Increased patient accountability
6.1.3.3. Facilitate smoother patient discharges
6.1.3.4. Employee Retention
6.1.4. IT Application Usefulness
6.1.4.1. Utilization Percentage
6.1.4.2. IT Team Demand for Troubleshooting and training
6.1.4.3. Job performance - Employee Evaluation
6.1.4.4. Vendor Evaluation
6.1.4.5. Third Party Payer Evaluation
7. IT Strategy
7.1. Goal
7.1.1. Reduce Costs for Hospital, Third Party Payers, and Patients
7.1.2. Improve Patient Satisfaction and Outcomes
7.1.3. Decrease Readmissions
7.1.4. Improve Job Satisfaction for Hospital Staff
7.1.5. Increase Access to Community Resources
7.2. Organizational Strategy
7.2.1. Glaser & Salzberg discuss the IT strategy in which, “strategy involves developing the IT ramifications of organizational initiatives, such as adding or changing services and products, growing market share, or improving service, streamlining processes, or reducing costs” (p. 678, 2011).
7.3. Business Demand
7.3.1. Hospitals are continuously challenged with managing costs while providing the best patient care possible, and the current dynamics within the national healthcare environment add an additional obstacle in delivering affordable care. Specifically within my hospital system, the need to reduce costs through the streamlining of processes is pivotal as our patient population creates a gross financial challenge due to a high volume of uninsured patients.
8. Strategic Vector
8.1. Organizational Goal: "continuous improvement of core operational processes and information management needs, determined by examining the role of new information technologies, and derived by assessment of strategic trajectories"(Glaser & Salzberg, 2011).
8.1.1. Materials
8.1.2. Personel
8.1.3. Services
8.1.4. Duration
8.2. Deriving IT agenda directly from the organization's goals and plans.
8.2.1. This program involves enhancing the area of EHR that manages patient discharges in order to improve the discharge process, advance continuity of care, reduce patient and hospital costs, and ensure more successful patient outcomes.
9. IT Assets
9.1. 1. Application Systems
9.1.1. Discharge Planning Tool
9.1.1.1. Improve discharge process
9.1.1.2. Program accessible to all involved parties, most importantly to patients. An article published in U.S. News stated, "Patient engagement has been dubbed by some experts as the next 'blockbuster drug,' and shared decision making is seen as the pinnacle of engaging and informing patients" (Gearen, 2013)
9.1.1.3. Online accessibility
9.2. 2. Data
9.2.1. Length of Stay
9.2.2. Hospital Readmissions
9.2.3. Employee Satisfaction scores
9.2.4. Patient Satisfaction scores
9.3. 3. IT staff
9.3.1. Program Developers
9.3.2. Project Manager
9.3.3. Trainers/Support Personnel
9.3.4. Department Leaders
9.4. Technical Architecture
9.4.1. EHR Integration
10. References
11. Vision Statement
11.1. My discharge planning tool will improve continuity of care during the discharge process by providing a platform for communication between all health care providers while allowing the patients to get involved and take ownership of their health. This will reduce hospital costs, improve the staff's efficiency, and ensure patient satisfaction.
12. User Experience
12.1. Powerpoint presentation of the Discharge Planning tool: PDAP presented to RN Case Manager
12.1.1. Feedback
12.1.1.1. "It sounds like a good idea, but she would be concerned that she wouldn’t be trained well enough and that she’d spend all of her time trying to figure out how to do her job with this new tool".
12.1.1.1.1. An IT staff would be hired specifically for the development, training, and troubleshooting of the program to best prepare staff.
12.1.1.1.2. Team Leaders would be assigned for onsite assistance for minor obstacles
12.1.1.2. "Doesn’t this seem like extra steps to do a job she is already doing"?
12.1.1.2.1. I shared information regarding the impact of the discharge tool on the cost for inpatient stay, average length of stay, and readmission rates. I explained that with this tool, multiple parties are involved to alleviate these associated obstacles and concerns and the result will be easier discharge planning.
12.1.1.2.2. We discussed the task requirements both with and without the discharge planning tool and the activity is different but not additional work. Actually, the tool creates a structure to efficiently manage the tasks at hand and once the staff is comfortable with the technology, the job will actually be completed with less steps.
12.1.1.3. "How does this benefit us RN Case Managers"?
12.1.1.3.1. I would start by discussing what struggles they have with discharges, and relate that to the struggles that the hospitals face with managing costs
12.1.1.3.2. By addressing the financial challenges of the hospital, we are all ensured more job security
13. Business Process Improvement
13.1. Patient Utilization
13.1.1. Are patients informed and educated on what resources are available to them?
13.1.2. Do patients appreciate being involved in the discharge process?
13.1.3. Patients are not accountable for follow through, how does this impact patient outcomes?
13.2. Employee Buy-In and Utilization
13.2.1. Is the staff using the tool?
13.2.2. Do the staff understand and appreciate the benefits as a result of the tool?
13.2.3. Are there best practices or suggestions to improve use?
13.3. Management Monitoring Employee Productivity
13.3.1. Is the staff utilizing the tool as requested?
13.3.2. Are outcomes improved?
13.3.3. Are tasks completed more efficiently or thoroughly?
13.4. Tool to Assess Effectiveness of Discharge Planning
13.4.1. Is communication between various parties improved?
13.4.2. Does the IT tool provide a useful platform for productive discharge planning?
13.4.3. Is continuity of care more fluent?
13.4.4. Are readmissions and length of stays reduced?
13.5. Continuity of Care
13.5.1. A platform for communication between inpatient and outpatient care providers will improve the transition to post-hospitalization care.
13.5.2. Vendors providing home care services will be able to document progress which will be accessible to all providers.
13.5.3. Third party payers can monitor the treatment plans and the progress from admission through the termination of care which will facilitate a smoother billing process.
14. Strategy Evolution
14.1. Continuous improvement of processes is integrated into this tool because information will always be updated and utilized according to best practices. Evaluation of current use, opportunity for feedback and suggestions, and revisions will be integral to the usefulness of this tool.
14.1.1. Example: My original proposal identified very few individuals as necessary during the earlier stages of this program, but in further discussing the details of this tool, I realize that I must revise my organizational structure to include more experienced professionals.

