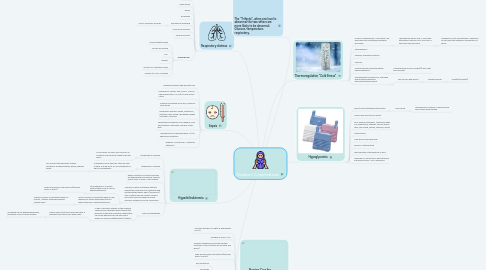
1. Sepsis
1.1. Prevention begins with prenatal care
1.2. Examples of causes: GBS, PROM, TORCH, Chorioamnionitis, UTI, but it could be any cause
1.3. Suspicious drainage from eyes, umbilical cord stump
1.4. Respiratory distress: apnea, retractions, grunting, nasal flaring, decreased oxygen saturation, cyanosis
1.5. Temperature instability, poor feeding, color abnormalities: petechiae, jaundice, pallor, grey
1.6. Hypoglycemia or hyperglycemia, N/V/D, abdominal distention
1.7. Requires IMMEDIATE IV antibiotic treatment
2. Hyperbilirubinemia
2.1. Physiological Jaundice
2.1.1. Occurs after 24 hours as a result of an immature liver trying to break down the RBC's
2.2. Pathological Jaundice
2.2.1. A disease process that can often be seen at birth. Can be do to RH incompatibility or ABO incompatibility.
2.2.1.1. Can result in the hemolytic anemia conditions: Erythroblastosis fetalis, hydrops fetalis.
2.3. Either condition can lead to bilirubin encephalopathy-kernicterus: toxicity, yellow stain on brain, if not treated.
2.4. Coombs Positive-Antibodies that act against the red blood cells, attacking and destroying the baby’s RBC’s (Hemolysis). This is determined by a direct coombs blood test from the newborn blood. Typically obtained from the cord blood.
2.4.1. If the newborn is Coombs Positive they more at risk for hyperbilirubinemia
2.4.1.1. Draw bili levels per unit protocol(typically every 12 hours)
2.4.2. Direct Coombs: a blood test drawn on the newborn to detect antibodies that act against the RBC's causing hemolysis.
2.4.2.1. Indirect Coombs: a blood test drawn on mother, detects antibodies against foreign RBC’s.
2.5. ABO incompatability
2.5.1. In ABO Hemolytic disease of the newborn maternal IgG antibodies pass through the placenta to the fetal circulation where they can cause hemolysis of the fetal RBC’s which can lead to fetal(hemolytic) anemia
2.5.1.1. Simply means that mom and baby have a different blood type from each other.
2.5.1.1.1. Increased risk for hyperbilirubinemia, especially if also coombs positive
3. Nursing Care for Hyperbilirubinemia
3.1. Typically less than 10 mg/dl is appropriate for D/C
3.2. Dangerous levels >13.0
3.3. Frequent feedings-to promote bilirubin excretion in stools (stools will be loose and green).
3.4. Draw bili levels per unit protocol(typically every 12 hours)
3.5. Phototherapy
3.5.1. Eye protection
3.5.2. Eye drops
3.5.3. No lotion while under lights
3.5.4. Change position q2 hrs.
3.5.5. Touch times/bonding
4. Respiratory distress
4.1. Grunting
4.2. Nasal flaring
4.3. Apnea
4.4. Tachypnea
4.5. Asymetrical breathing
4.5.1. Use of accessory muscles
4.6. Circumoral cyanosis
4.7. Central cyanosis
4.8. Nursing Care
4.8.1. Ensure patent airway
4.8.2. Suction as needed
4.8.3. PPV
4.8.4. Oxygen
4.8.5. Monitor O2 saturation levels
4.8.6. Transfer to NICU if needed
5. The "Trifecta", when one level is abnormal the two others are more likely to be abnormal: Glucose, temperature, respiratory.
6. Thermoregulation "Cold Stress"
6.1. A baby in hypothermia, “cold stress” will have difficulty maintaining metabolic processes
6.1.1. Temperature below 36.5 C. Neonates extremities may feel cool, the core of the body may feel warm
6.1.1.1. Shivering is not a manifestation. Newborns do not have the metabolic mechanisms to shiver
6.2. Hypoglycemia
6.3. Hypoxia, respiratory distress
6.4. Acidosis
6.5. Nursing care to achieve/maintain thermoregulation
6.5.1. If temperature is WDP: blanket(s) and a hat are sufficient
6.6. If temperature is below 36.5, intervene with a thermoregulatory intervention/environment
6.6.1. Skin to skin with parent
6.6.1.1. Radiant warmer
6.6.1.1.1. Isolette(incubator)
7. Hypoglycemia
7.1. GDM/LGA/SGA/preterm/post-term
7.1.1. More at risk
7.1.1.1. Hypoglycemic Protocol: check glucose level before each feeding
