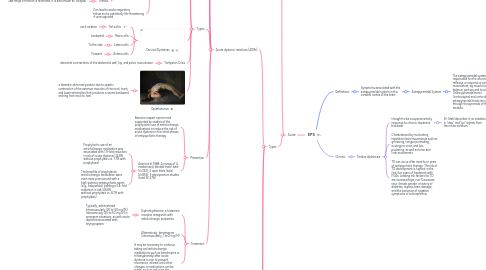
1. Acute
1.1. It is estimated that approximately 50% of patients treated with high-potency FGAs (such as haloperidol) develop acute EPS within the first several days of treatment
1.2. Types
1.2.1. Acute dystonic reactions (ADRs)
1.2.1.1. Definition
1.2.1.1.1. sustained muscle contraction producing involuntary, abnormal postures, often in a twisting nature affecting the trunk, neck, face, and extremities
1.2.1.1.2. Symptoms typically occur shortly after administration of an antipsychotic.
1.2.1.2. Epidemiology
1.2.1.2.1. The prevalence of ADRs varies by population, time period, and medication.
1.2.1.2.2. ADRs occur in a range of 3%-10%, but analysis of pooled data indicates they are as high as 51.2% with high-potency antipsychotics.
1.2.1.2.3. FGAs are more likely to cause adverse reactions than SGAs.
1.2.1.3. Risk factors
1.2.1.3.1. Young age and male gender, history of substance abuse, and family history of dystonia.
1.2.1.3.2. Acute dystonia is common with FGAs such as haloperidol and less common with SGAs.
1.2.1.4. Types
1.2.1.4.1. Oculogyric Crisis
1.2.1.4.2. Laryngeal Dystonia
1.2.1.4.3. Cervical Dystonias
1.2.1.4.4. Tortipelvis Crisis
1.2.1.4.5. Opisthotonus
1.2.1.5. Prevention
1.2.1.5.1. Based on expert opinion and supported by studies of the prophylactic use of anticholinergic medications to reduce the risk of acute dystonia in the initial phases of antipsychotic therapy.
1.2.1.5.2. Arana et al. 1988: A review of 4 randomized, blinded trials (total N=232); 2 open trials (total N=856); 3 retrospective studies (total N=278)
1.2.1.6. Treatment
1.2.1.6.1. Diphenhydramine, a histamine receptor antagonist with anticholinergic properties
1.2.1.6.2. Alternatively, benztropine (intramuscularly, 1 to 2 mg IM)
1.2.1.6.3. It may be necessary to continue taking oral anticholinergic medications such as benztropine or trihexyphenidyl after acute dystonia is over to prevent recurrence, at least until other changes in medications can be made, such as reducing the dosage of medication or switching to an antipsychotic medication less likely to cause acute dystonia.
1.2.2. Akathisia
1.2.2.1. Subjective feeling of internal restlessness accompanied by a persistent urge to move, which leads to repetitive movements such as leg crossings, swings, or shifting from one foot to another
1.2.2.2. The condition is very common (about half of all cases of EPS), poorly understood, and difficult to treat. It usually happens in the first three months.
1.2.2.3. About 25% of patients treated with FGAs develop akathisia, but it also occurs with SGAs.
1.2.2.4. Treatment
1.2.2.4.1. Options include antipsychotic dose reduction, liposoluble beta adrenergic blockers, and benzodiazepines
1.2.2.4.2. Anticholinergic medications do not work for akathisia
1.2.3. Parkinsonism
1.2.3.1. Commonly manifests as tremor, skeletal muscle rigidity, and/or bradykinesia
1.2.3.2. Risk factors for this type of Parkinsonism are age (elderly), gender (females), cognitive deficit, and early onset EPS.
1.2.3.3. Parkinsonism caused by antipsychotics is reversible, but its duration is variable.
1.2.3.4. Parkinsonism can occur within days to months after starting antipsychotics.
1.2.3.5. Treatment
1.2.3.5.1. Treatment of choice has not been established, but dose reduction and anticholinergic drugs may be helpful.
2. Definitions
2.1. Symptoms associated with the extrapyramidal system in the cerebral cortex of the brain
2.1.1. Extrapyramidal System
2.1.1.1. The extrapyramidal system is responsible for the unconscious, reflexive or responsive control of musculature, eg muscle tone, balance, posture and locomotion. Unlike pyramidal tracts (corticospinal and corticobulbar), extrapyramidal tracts do not travel through the pyramids of the medulla.
3. Chronic
3.1. Tardive dyskinesia
3.1.1. thought to be a supersensitivity response to chronic dopamine blockade
3.1.1.1. Dr. Stahl describes it, as imbalance in “stop” and “go” signals from the motor striatum
3.1.2. Characterized by involuntary, repetitive facial movements such as grimacing, tongue protruding, oculogyric crisis, and lips puckering, as well as torso and limb movements
3.1.3. TD can occur after months or years of antipsychotic therapy. The risk of TD development is highest in the first five years of treatment with FGAs. Leading risk factors for TD are increased age, non-Caucasian race, female gender, a history of diabetes, organic brain damage, and the presence of negative symptoms of schizophrenia.
