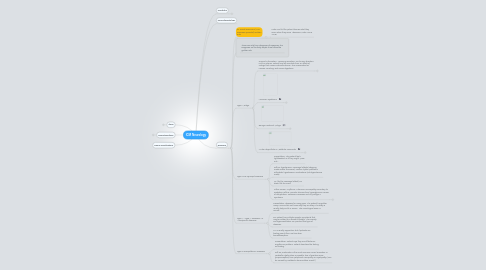
1. Sleep
1.1. Sleep over the lifespan
1.2. Normal Sleep Cycles
1.2.1. Stage I
1.2.2. Stage II
1.2.3. Stage III and Stage IV
1.3. REM Behavior Disorder
1.4. Charles Bonnet Syndrome
1.5. Severe Obstructive Sleep Apnea (OSA)
1.6. Temporal Lobe Seizures- Secondary to (OSA)
2. Neurotoxicology
2.1. Neurotoxins Types
2.1.1. Elemental
2.1.2. Radiation
2.1.3. Botanical
2.1.4. Biological
2.2. Establishign Neurotoxicity Causes
2.2.1. Exposure
2.2.2. Temporality
2.2.3. Dose-response relationship
2.2.4. Improvement after removal from exposure
2.2.5. Clinical features consistent w/ other cases
2.2.6. Other causes eliminated
2.3. Thallium Poisoning
2.3.1. Neuro Exam
2.3.1.1. Hypesthesia in feet, decreased proprioception feet/hands, decreased vibratory sense feet/hands, normal motor strength/ not muscle wasting, and decreased ankle jerks.
2.3.2. Dx workup
2.3.2.1. CBC (lab test), and Nerve conduction study
2.3.2.1.1. results of nerve conduction study shows peripheral neuropathy in the legs are greater than the neuropathy in the arms.
2.3.2.2. Clinical presentation
2.3.2.2.1. Symptoms are progressive, several co-workers have similar symptoms, and the PATIENT'S HAIR IS FALLING OUT! (14days post onset of symptoms and hair was completely gone at 3 weeks)
2.3.2.3. Elevated thallium in 24hr urine sample, blackened hair roots, patient develops alopecia, common source of exposure (i.e. coffee pots at patient's job).
2.3.3. In general, thallium poisoning causes a toxic peripheral neuropathy. Toxic metabolic cuases of neuropathy are very common. The onset is days to weeks. The earliest symptoms present in the lower extremities. EMG can show normal to mildly slow motor conduction. Patient are slow to recover. Take home: Toxins takes days to week for symptoms to show... longer than acute neuropathy (infarct) and shorter than malignancy or chronic problem.
2.4. Alprasolam Overdose
2.4.1. Clinical Case: 24yo man brought into ER after a tonic clonic seizure. At the bedside his girlfriend suffers a tonic clonic seizure resulting in a scalp laceration and as loss of bowel/bladder control.
2.4.1.1. PMH: none for both; Medications: both deny any meds; Social Hx: both smoked marijuana 2 days prior to seizure onset and otherwise denies alcohol or other drugs. Occupational Hx: man places vinyl siding, and the woman doesn't work.
2.4.1.2. PE: vitals-normal; HEENT- normal except 3cm scalp laceration on woman; OP- clear; CV- regular rate/rhythm; ABD- soft/non tender + BS; and skin- no track marks.
2.4.1.2.1. Neuro Exam
2.4.2. Unique Feature of a Seizure: a seizure lowers the neuronal depolarization threshold making it easier for a neuron to access a firing event.
2.4.3. Receptors
2.4.3.1. Glutamate (NMDA) Receptors
2.4.3.1.1. Glutamate Agonists
2.4.3.2. GABA Receptors
3. Neuro-complications
4. Headache
4.1. Tension Headache
4.1.1. Presentation: headache for many days and gets worse as the day goes on.
4.1.2. Tx: Good diet, sleep, exercise, low stress
4.1.3. This headache is usually induced by stress. Commonly found in persons under a great amount of stress; occupational, school, etc.
4.2. Aneursym or Meningitis
4.2.1. Presentation: "Worst headache of my life", focal neurological symptoms. If new onset immunocompromised patient or if the headache is daily this is possibly an EMERGENCY.
4.3. Migraine
4.3.1. Presentation: onset more than one month prior or a year prior. Has a prodrome usually a visual disturbance of some sort (aura). Can also have nausea aura prior to headache symptoms. Patient experiences abnormal cognitive function, and should not do very difficult work while having a migraine. note: as the aura passes the headache gains strength gradually.
4.3.1.1. Visual Aura: fortification spectra, shimmering lights, visual field loss.
4.3.1.2. Some patients have aura but NO headache. This is called Migraine Equivalent. (Dr. Vasko actually has this.)
4.3.2. Diagnostic features: Unitemporal headache that usually starts in the occipital region (near the visual field) and marches to the frontal lobe and some focal deficits may be appreciated. These can caused by hormonal imbalance, sugary foods (candy, chocolate), MSG, stress, lack of sleep, and lack of exercise.
4.3.3. Treatment: Beta-blockers (propanolol; low dose), seizure meds (calcium channel blockers; low dose), low dose TCAs (Amitryptiline-weight gain side effect), Topiramate- weight loss side effect; Tryptans-work on serotonin system. Can take periodically for rescue w/ migraine.
4.3.4. Types:
4.3.4.1. Migraine without aura
4.3.4.2. Migraine w/ aura
4.3.4.3. Migraine w/ extended aura
4.3.4.4. Migraine w/ aura and infarction
4.4. Chronic Paroxysomal Hemicrania
4.5. Cluster Headache
4.6. Carotid Dissection
4.7. Psuedotumor Cerebri
4.8. Aneursym of PComm
4.9. Benign Exertional Headache
4.10. Giant Cell Arteritis
4.11. Glioblastoma Multliforme
5. Neurodermatology
6. Dizziness
6.1. Dr. David Dracman's (M.D. Dizziness Specialist) Golden Rule
6.1.1. Listen and let the patient discuss what they mean when they same "dizziness"! Take YOUR TIME!
6.2. There are only four categories of Dizziness! The Diagnosis can be fairly simple if we follow the golden rule.
6.3. Type I Vertigo
6.3.1. General Information: "spinning sensation, can be any direction, mild or intense. Patient may be immobile from an attack of vertigo that causes motions sickness. This is associated w/ nausea, vomiting, and severe dysphoria.
6.3.1.1. The pathology of vertigo can be"peripheral/otological" (98%). More intense and acute vertigo symptoms are more likely to be peripheral and less serious.
6.3.1.2. The pathology of vertigo can be a "central/brainstem" lesion (2%) or cerebellar stroke. (Note: central vertigo tends to be less severe "vertigo symptoms" than otologic vertigo and are usually associated w/ other symptoms.
6.3.2. Meniere's Syndrome
6.3.2.1. Presentation: recurrent episodes of intense vertigo, tinnitus, hearing loss, and fulling in the head or ears. Usually brought on by eating a high salt diet. The vertigo is not invoked by being in any position. It is constant and does not get better or worse by lying down or sitting up.
6.3.2.2. Pathogenesis: increased endolymph causing swelling of the labyrinth ductal system.
6.3.2.3. Causes: genetic causes, trauma, infectious, autoantibodies, and increased salt intake. Can also be brought on by alcohol and high blood pressure.
6.3.2.4. Tx: low salt diet, low dose hydrocholorthiazide (HCTZ), and good sleep hygiene.
6.3.3. Benign Positional Vertigo
6.3.3.1. Presentation: "Twirling of the world around me". Every time the patient moves the vertigo gets worse. The patient cannot get out of bed. The patient is afraid and feels as if they are going to die. No tinnitus is present. This patient is usually older.
6.3.3.2. Pathogenesis: Small otoliths from the saccule get into the semilunar canals of one ear and displace stereocilia. This causes unilater activation of the vestibular complex which is read by the brain as motion turning toward the affected ear; however, this is an illusion.
6.3.3.3. Tx: Clear out the debris from the semicircular canals using the Epley maneuver-position and rotation of the head.
6.3.3.3.1. Epley maneuver works in 50% of patients.
6.3.4. Acute Labyrinthitis or Vestibular Neuronitis
6.3.4.1. Presentation: The patient has a upper respiratory infection, during which or shortly thereafter developing intense vertigo. This last a few days and tends not to recur.
6.3.4.2. KEYNOTE FEATURE: IT does NOT affect Hearing!
6.3.4.3. Tx: use meclizine (Antivert) 25mg/6hrs, Phenergan (IV) 25mg, or diazepam (Valium) I.V. or Oral works in minutes time. Works the best! A short course of steroids are also helpful.
6.4. Type II Pre-Syncopal Dizziness
6.4.1. Presentation: The patient feels lightheaded, as if they might "pass out".
6.4.2. Diff Dx: hypotension, vasovagal attacks (skipping meals makes this worse), cardiac rhythm problems, orthostatic hypotension, medications (anti-hypertensive meds)
6.4.3. Tx: (for the vasovagal attack) Lie down flat for 5mins
6.4.4. Other causes: Arrythmia, Autonomic neuropathy secondary to Diabetes Mellitus, Osmotic diuresis from hyperglycemic causes of dehydration, Parkinson's Disease and Chy Drager's Syndrome
6.4.4.1. Chy Drager's Syndrome
6.4.4.1.1. Multiple-system atrophy (MSA) is a degenerative neurological disorder. MSA is associated with the degeneration of nerve cells in specific areas of the brain. This cell degeneration causes problems with movement, balance, and other autonomic functions of the body such as bladder control or blood-pressure regulation. The cause of MSA is unknown and no specific risk factors have been identified. Around 55% of cases occur in men, with typical age of onset in the late 50s to early 60s. MSA often presents with some of the same symptoms as Parkinson's disease. However MSA patients generally show minimal if any response to the dopamine medications used for Parkinsons.
6.5. Type IV "Type IV Dizziness" or "nonspecific dizziness"
6.5.1. Presentation: dizziness for many years. The patient has gotten many MRIs and do not know why they are dizzy. The dizzy is usually daily and it is severe. The neurological exam is normal.
6.5.2. Dx: Patient has multiple somatic complaints that may be related to a stressful lifestyle. Also anxiety and hyperventilation can produce this type of dizziness.
6.5.3. Tx: is usually supportive, but if patients are feeling poorly then use low dose benzodiazapines.
6.6. Type III Disequilibrium Dizziness
6.6.1. Presentation: Patient says they are off balance- equilibrium problem. Patient describes the feeling as floating.
6.6.2. Diff Dx; medicaiton is the most common cause, brainstem or cerebellar dysfunction is possible, loss of position sense (proprioception) from peripheral neuropathy or myelopathy. (Can be caused by metabolic abnormalities as well.)
