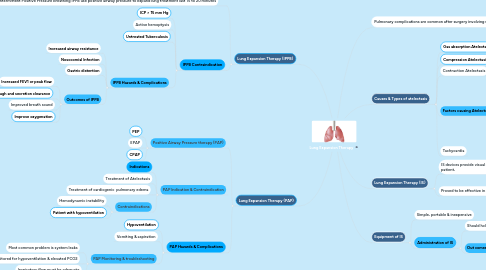
1. Pulmonary complications are common after surgery involving upper abdomen or thorax
1.1. Atelectasis
1.1.1. Pneumonia
1.1.1.1. Acute Respiratory Failure
1.2. is utilized to prevent or correct respiratory complications in postoperative period.
2. Causes & Types of atelectasis
2.1. Gas absorption Atelectasis
2.2. Compression Atelectasis
2.3. Contraction Atelectasis
2.4. Factors causing Atelectasis
2.4.1. Neuromuscular disorders
2.4.2. Surgery near diaphragm
2.4.3. Poor cough
2.4.4. Clinical sign of Atelectasis
2.4.4.1. Tachapnea
2.4.4.2. Fine, Late- inspiratory crackels
2.4.4.3. Increased density & signs of volume loss in chest
2.5. Tachycardia
3. Lung Expansion Therapy (IS)
3.1. IS devices provide visual cause to patient,
3.2. Proved to be effective in high risk patients.
3.2.1. Indications for Incentive Spirometry
3.2.1.1. Presence of pulmonary Atelectasis
3.2.1.2. Presence of a restrictive lung defect associated with quadriplegia or dysfunctionl diaphragm
4. Equipment of IS
4.1. Simple, portable & inexpensive
4.2. Administration of IS
4.2.1. Should hold breathing for 5 to 10 second
4.2.2. Out comes of IS
4.2.2.1. Absence or improvement in sign of Atelectasis
4.2.2.2. Increased Spo2
4.2.2.3. Improved inspiratory muscle performance & cough
5. Lung Expansion Therapy (IPPB)
5.1. Intermittent Positive Pressure breathing IPPB use positive airway pressure to expand lung treatment last 15 to 20 minutes
5.1.1. Indications for IPPB
5.1.1.1. Patient with Atelectasis not responsive to other modalities such as IS
5.2. IPPB Contraindication
5.2.1. ICP > 15 mm Hg
5.2.2. Active hemoptysis
5.2.3. Untreated Tuberculosis
5.2.4. IPPB Hazards & Complications
5.2.4.1. Increased airway resistance
5.2.4.2. Nosocomial Infection
5.2.4.3. Gastric distention
5.2.4.4. Outcomes of IPPB
5.2.4.4.1. Increased FEV1 or peak flow
5.2.4.4.2. Enhance cough and secretion clearance
5.2.4.4.3. Improved breath sound
5.2.4.4.4. Improve oxygenation
6. Lung Expansion Therapy (PAP)
6.1. Positive Airway Pressure therapy (PAP)
6.1.1. PEP
6.1.2. EPAP
6.1.3. CPAP
6.2. PAP Indication & Contraindication
6.2.1. Indications
6.2.2. Treatment of Atelectasis
6.2.3. Treatment of cardiogenic pulmonary edema
6.2.4. Contraindications
6.2.4.1. Hemodynamic instability
6.2.4.2. Patient with hypoventilation
6.3. PAP Hazards & Complications
6.3.1. Hypoventilation
6.3.2. Vomiting & aspiration
6.3.3. PAP Monitoring & troubleshooting
6.3.3.1. Most common problem is system leaks
6.3.3.2. Patient must be monitored for hypoventilation & elevated PCO2
6.3.3.3. Inspiratory flow must be adequate

