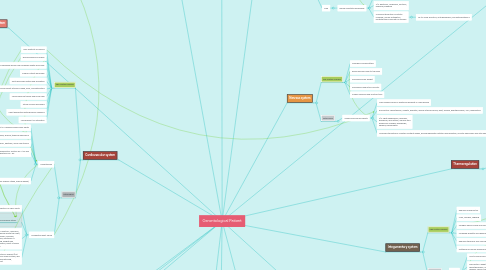
1. Intelligence
1.1. Age related changes
1.1.1. Crystallized intelligence maintained
1.1.2. Fluid intelligence decreases
1.1.3. Basic intelligence is maintained
2. Musculoskeletal system
2.1. Age related changes
2.1.1. Impaired flexion and extension movements
2.1.2. Slight wrist flexion
2.1.3. Slight kyphosis
2.1.4. Shortening of vertebrae
2.1.5. Between ages 20 and 70, height decreases approximately 2 inches
2.1.6. Bones more brittle
2.1.7. Slight knee flexion
2.1.8. Decrease in bone mass and bone mineral
2.2. Pathologies
2.2.1. Osteoarthritis
2.2.1.1. Progressive degeneration and abrasion of joint cartilage, with 5e formation of new bone at the joint surface
2.2.1.2. Effects most people over 55 to some extent
2.2.1.3. Risk factor: disequilibrium between destructive and synthetic elements leads to a lack of homeostasis necessary to maintain cartilage, causing joint changes. Excessive use of joint, trauma, obesity, low vitamin d and c, genetic factors, acromegaly,
2.2.1.4. S/S: crepitus of the joints, discomfort at the joint with extended use
2.2.1.5. Nursing interventions: rest, heat/ice, t’ai chi, aqua therapy, gentle massage, splints, braces, canes, weight reduction, occupational and physical therapy, arthroplasty-joint replacement
2.2.1.5.1. Medications: analgesics to control pain
2.2.1.5.2. Diet: abundance of cold water fish and other foods high in essential fatty acids, vitamin a, b, b6, c, and e. Zinc, selenium, niacin-amide, calcium, magnesium
3. Urinary system
3.1. Age related changes
3.1.1. Decreased bladder capacity
3.1.2. Decreased size of renal mass
3.1.3. Decreased tubular function
3.1.4. Decrease in nephrons
3.1.5. Between ages 20 and 90 renal blood flow decreases 53%, and glomerular filtration rate decreases 50%
3.1.6. Weaker bladder muscles
3.2. Pathologies
3.2.1. Urinary tract infection
3.2.1.1. Most common infection of older adults
3.2.1.2. Risk factors:
3.2.1.2.1. Poor hygiene, improper cleaning after bowel elimination, low fluid intake, excessive fluid loss, hormonal changes, catheter
3.2.1.2.2. Escherichia coli (women), proteus (men)
3.2.1.3. S/S: burning, urgency, fever, retention, incontinence, hematuria
3.2.1.4. Diagnostic: Bacteriuria- >105
3.2.1.5. Nursing interventions: adequate urinary drainage, I&O’s, fluids, cranberry juice, avoid urinary catheter
3.2.2. Urinary incontinence
3.2.2.1. Common and bothersome disorder of older adults, in more than half of institutionalized older population
3.2.2.2. Risk factors: delirium, dementia, cerebrovascular accident, diabetes mellitus, congestive heart failure, UTI
3.2.2.2.1. medications that can affect continence: diuretics, antianxiety agents, antipsychotics, antidepressants, sedatives, narcotics, antiparkinson agents, antispomodics, antihistamine, calcium channel blockers, alpha-blockers, alpha-stimulants
3.2.2.3. Symptoms: urgency, burning, vaginal itching, pain, pressure in bladder area, fever
3.2.2.4. Nursing interventions: refer patient for a comprehensive medical evaluation, assess activities of daily living, note degree of dependency
4. Gastrointestinal system
4.1. Age related changes
4.1.1. Slower peristalsis
4.1.2. Fewer cells on absorbing surface of intestines
4.1.3. Less production of HCL, pepsin, lipase, and pancreatic enzymes
4.1.4. Decreased stomach motility and hunger contractions, and emptying time
4.1.5. Atrophy of gastric mucosa
4.1.6. Decrease esophageal motility
4.1.7. Decreased taste sensation
4.1.8. Esophagus more dilated
4.1.9. Reduced saliva and salivary ptyalin
4.1.10. Liver smaller in size
4.1.11. Reduced intestinal blood flow
4.2. Pathologies
4.2.1. Hiatal hernia
4.2.1.1. Affects about half of the people in the US over age of 50, more common in women
4.2.1.2. Risk factors: low-fiber diet, GERD, obesity
4.2.1.3. S/S: heartburn, dysphagia, belching, vomiting, regurgitation, pain, and bleeding
4.2.1.4. Diagnostics: barium swallow and esophagoscopy
4.2.1.5. Nursing interventions: weight reduction, bland diet, milk, several small meals, avoid eating before bedtime, sleep in slight recombinant position
4.2.1.5.1. Medications: antacids, H2 blockers, proton pump inhibitor
4.2.2. Colorectal cancer
4.2.2.1. Cancer along large intestine is common with advancing age
4.2.2.2. Diagnostics: colonoscopy with biopsy and CT colonoscopy, fecal occult blood testing
4.2.2.3. S/S: rectal bleeding, bloody stools, change in bowel pattern, feeling of incomplete emptying of bowel, anorexia, nausea, abdominal discomfort, pain over affected region, weakness, fatigue, unexplained weight loss, anemia
4.2.2.4. Nursing interventions: preparation for surgery, have regular meals, restrict tea and coffee, reduce alcohol and carbonated drinks, eat something solid with each meal
4.2.2.4.1. Radiotherapy: can downstage tumor to aid complete excision
4.2.2.4.2. Surgical resection
4.2.2.4.3. Chemotherapy: with high-risk Dukes B or Dukes C tumors with nodal disease to reduce recurrence
5. Cardiovascular system
5.1. Age related changes
5.1.1. Less elasticity of vessels
5.1.2. Blood pressure increases
5.1.3. Resistance to peripheral blood flow increases slightly each year
5.1.4. Cardiac output decreases
5.1.5. Aorta becomes dilated and elongated
5.1.6. More prominent arteries in head, neck, and extremities
5.1.7. Valves become thicker and more rigid
5.1.8. Stroke volume decreases
5.1.9. Heart pigmented with lipofuscin granules
5.1.10. Less efficient O2 utilization
5.2. Pathologies
5.2.1. Hypertension
5.2.1.1. Most prevalent CV disease among older adults
5.2.1.2. Causes: vasoconstriction, peripheral resistance, hyperthyroidism, Parkinson disease, Paget’s disease, anemia, thiamine deficiency
5.2.1.3. S/S: high blood pressure, awakening with a dull headache, impaired memory, disorientation, confusion, epistaxis, and a slow tremor
5.2.1.4. Diagnostics: systolic bp >140 and diastolic bp > 90
5.2.1.5. Nursing interventions: rest, reduce sodium intake, reduce weight,
5.2.1.5.1. Nonpharmocologic measures advised: biofeedback, yoga, meditation, relaxation exercises, fish oil supplements, garlic, hawthorn berries, Rauwolfia, periwinkle, increase whole grain in diet
5.2.1.5.2. DASH Diet: rich in fruits, veggies, whole grain, low-fat dairy foods
5.2.1.5.3. Medications:
5.2.2. Congestive heart failure
5.2.2.1. Leading cause of hospitalization of older adults
5.2.2.2. Causes: arteriosclerotic heart disease, coronary artery disease, hypertension, diabetes mellitus, dyslipidemia, sleep-disordered breathing, albuminuria, Anemia, chronic kidney disease, illicit drug use, sedentary lifestyle, psychological stress
5.2.2.3. S/S: dyspnea on exertion, confusion, insomnia, wandering during the night, agitation, depression, anorexia, nausea, weakness, shortness of breath, wheezing, weight gain, bilateral ankle edema, moist crackles on auscultation
5.2.2.4. Nursing interventions: bedrest (not complete), reduce sodium intake, skin care, frequent repositioning, emotional support
5.2.2.4.1. Medication: ACE inhibitor, beta blocker, digitalis, diuretics
6. Respiratory system
6.1. Age related changes
6.1.1. Thoracic muscles more rigid
6.1.2. Reduced basilar inflation
6.1.3. Alveoli fewer in number and larger in size
6.1.4. By age 90 years, approximately 50% increase in residual capacity
6.1.5. Blunting of cough and laryngeal reflexes
6.1.6. PO2 reduced as much as 15% between ages 20 and 80
6.1.7. Loss of elasticity and increased rigidity
6.1.8. Decreased ciliary action
6.1.9. Forced expiratory volume reduced
6.2. Pathologies
6.2.1. Pneumonia
6.2.1.1. Common among older adults, one of the leading causes of death in age group
6.2.1.2. Risk factors: shallow breathing, poor chest expansion, high prevalence of respiratory diseases, lowered resistance to infection, reduced sensitivity of pharyngeal reflexes
6.2.1.3. Causes: Streptococcus pneumonia, gram negative bacilli, anaerobic bacteria, and influenza
6.2.1.4. S/S: pleuritic pain, minimal fever, slight cough, fatigue, rapid respirations, confusion, restlessness
6.2.1.5. Diagnostics: chest x-ray, chest auscultation, ABG levels
6.2.1.6. Nursing interventions: pneumonococcal vaccine, hydration-IV fluids, higher calorie intake, monitor oxygen saturation, oxygen therapy if needed, rest to conserve energy
7. Cells
7.1. Age related changes
7.1.1. Intracellular fluid is decreased
7.1.1.1. Leads to less total body fluid
7.1.1.1.1. Risk for dehydration
7.1.2. Bone mass decreases
7.1.3. Fat tissue increases until sixth decade of life
7.1.4. Lean body mass reduced
7.1.5. Fewer functional cells in the body
7.1.6. Number of cells gradually reduced
8. Changes to the mind
8.1. Age related changes
8.1.1. Learning
8.1.1.1. Motivation changes
8.1.1.2. Delayed transmitting of information to the brain
8.1.2. Memory
8.1.2.1. Retrieval of information from long-term memory can be slowed
8.1.2.2. Sensory only lasts a few seconds
8.1.2.3. Working memory function is reduced
8.1.3. Personality
8.1.3.1. Consistent with how it was in earlier years
8.2. Pathologies
8.2.1. Dementia
8.2.1.1. Irreversible, progressive impairment of cognitive function affecting memory, orientation, judgment, reasoning, attention, language and problem solving
8.2.1.2. Alzheimer’s Disease
8.2.1.2.1. Most common form of dementia
8.2.1.2.2. Neurotic plaque with deposits of beta-amyloid protein, when clumping it impairs the function of nerve cells in the brain
8.2.1.2.3. Neurofibrillary tangles in the cortex, microtubules disintegrate and collapse the neuron transport system
8.2.1.2.4. Risk factors: Down syndrome, environmental and genetic factors, lipidemia, hypertension, smoking, head injury, mental and physical inactivity
8.2.1.2.5. S/S: changes in intellectual ability, anxious or depressed, language disturbances, visual disturbances, feeling of not being able to control limbs
8.2.1.2.6. Diagnostics: brain scan that reveals changes in brain structure, neurophysiology testing to evaluate cognition
8.2.1.2.7. Nursing interventions: estrogens role in prevention is being researched more, antioxidants, anti-inflammatory agents, folic acid/b12/b6 supplements, gene therapy to add nerve growth factor, medication to break down acetylcholine (donepezil, rivastigmine, galantamine)
9. Physical Appearance
9.1. Age related changes
9.1.1. Narrowing gait in women and wider gait in men
9.1.2. Deepening of hollows of axillae and intercostal and supraclavicular spaces
9.1.3. Darkening and wrinkling of skin around orbits
9.1.4. Thicker hair in ears and nose
9.1.5. Graying and thinning of hair
9.1.6. Ectropion of eyelids
9.1.7. Elongated ears
9.1.8. Arcus senilis
9.1.9. Growth of facial hair in women
9.1.10. Diminished muscle mass and skinfold thickness
9.1.11. Decreased height
10. Thermoregulation
10.1. Age related changes
10.1.1. Impaired sweating mechanism
10.1.1.1. More susceptible to heat stress
10.1.2. Reduced ability to respond to cold temperatures
10.1.3. Lower temperature
11. Endocrine system
11.1. Age related changes
11.1.1. Pancreases
11.1.1.1. Delayed and insufficient release of insulin
11.1.1.2. Reduced ability to metabolize glucose
11.1.2. Pituitary gland
11.1.2.1. Decreases in volume by 20%
11.1.2.2. Gonadal secretions decrease
11.1.3. Adrenal cortex
11.1.3.1. ACTH secretion decreases
11.1.3.2. Secretion of glucocorticoids is reduced
11.1.4. Thyroid gland
11.1.4.1. Fibrosis
11.1.4.2. Cellular infiltration
11.1.4.3. Lower BMI
11.1.4.4. Reduced radioactive iodine uptake
11.2. Pathologies
11.2.1. Hypothyroidism
11.2.1.1. Condition increases in prevalence with age
11.2.1.2. S/S: fatigue, weakness, disinterest in activities, anorexia, weight gain and puffy face, impaired hearing, peri orbital edema, constipation, cold intolerance, ataxia, paresthesia, dry skin, and coarse hair
11.2.1.3. Diagnostics: blood test TSH, T4 levels
11.2.1.4. Nursing Interventions: synthetic T4 replacement, treat and prevent signs and symptoms ( constipation, wear extra clothes if cold intolerant)
12. Integumentary system
12.1. Age related changes
12.1.1. Reduced melanocytes
12.1.2. Lines, wrinkles, sagging
12.1.3. Collagen fibers coarse and more random, reducing elasticity of the skin
12.1.4. Increased quantity and degeneration of elastin fibers
12.1.5. Reduced thickness and vascularity of the dermis
12.1.6. Flattening of dermal-epidural junction
12.2. Pathologies
12.2.1. Pruritus
12.2.1.1. Most common skin disease among older adults
12.2.1.2. Risk factors: diabetes, arteriosclerosis, hyperthyroidism, uremia, liver disease, cancer, pernicious anemia
12.2.1.3. S/S: uncomfortable, irritating sensation that makes you want to scratch
12.2.1.4. Nursing interventions: bath oils, moisturizing lotions, massage, vitamin supplements and diet high in vitamins, zinc oxide
12.2.1.4.1. Medications: antihistamines and topical steroids
13. Immune system
13.1. Age related changes
13.1.1. Inflammatory response declines
13.1.2. IgM concentration lower, IgA and IgG are higher
13.1.3. Large decline in cell-mediated immunity
13.1.4. T-cell activity declines and more immature T cells are present in the thymus
13.1.5. Immunosenescence- depressed immune response
13.1.5.1. Increases risk for infection
14. Sensory organs
14.1. Age related changes
14.1.1. Vision
14.1.1.1. Presbyopia
14.1.1.2. Stiffening of muscle fibers of lens
14.1.1.3. Visual field narrows
14.1.1.4. Pupillary sphincter hardens
14.1.1.5. Light perception threshold increases
14.1.2. Hearing
14.1.2.1. Atrophy of hair cells of organ of corti
14.1.2.2. Tympanic membrane sclerosis and atrophy
14.1.2.3. Increased cerumen and concentration of keratin
14.1.3. Taste and smell
14.1.3.1. High prevalence of taste impairment
14.1.3.2. Impaired ability to identify and discriminate among odors
14.1.4. Touch
14.1.4.1. Reduced tactile sensation
14.2. Pathologies
14.2.1. Cataracts
14.2.1.1. Clouding of the lens or its capsule causes the lens to lose its transparency
14.2.1.2. Common among older people
14.2.1.3. Risk factors: UV B rays exposure, diabetes, cigarette smoking, high alcohol consumption
14.2.1.4. S/S: no discomfort or pain, vision distorted, decreased night vision, blurred objects, feel like there is a film over eye, lens is yellow or yellow-brown, improvement in ability to see small print and objects
14.2.1.5. Treatment: surgery to remove lens, if only one eye effected then focus on strengthening vision that exists, sunglasses, shear curtains over windows, multiple soft lights instead of one bright one
15. Nervous system
15.1. Age related changes
15.1.1. Changes in sleep pattern
15.1.2. Reduced blood flow to the brain
15.1.3. Decreased brain weight
15.1.4. Decreased conduction velocity
15.1.5. Slower response and reaction time
15.2. Pathologies
15.2.1. Cerebrovascular accidents
15.2.1.1. Third leading cause of death and disability in older people
15.2.1.2. Risk factors: hypertension, obesity, diabetes, severe arteriosclerosis, gout, anemia, hypothyroidism, TIAs, dehydration
15.2.1.3. S/S: light-headedness, dizziness, headache, drop attack, memory and behavioral changes, hemiplegia, aphasia, hemianopsia
15.2.1.4. Nursing interventions: maintain a patent airway, provide adequate nutrition and hydration, monitor neurologic and vital signs, prevent complications associated with immobility, frequent skin care, frequent turns
16. Reproductive system
16.1. Age related changes
16.1.1. Male
16.1.1.1. Possible reduction in sperm count
16.1.1.2. Fluid-retaining capacity of seminal vesicles reduces
16.1.1.3. Venous and arterial sclerosis of the penis
16.1.1.4. Prostate enlarges in most men
16.1.2. Female
16.1.2.1. Flattening of labia
16.1.2.2. Drier, less elastic vaginal canal
16.1.2.3. Cervix becomes smaller
16.1.2.4. Ovaries become thicker and smaller
16.1.2.5. Fallopian tube atrophy and shortens
16.1.2.6. Endocervical epithelium atrophies
16.1.2.7. Uterus becomes smaller in size
16.1.2.8. Endometrium atrophies
16.1.2.9. More alkaline vaginal environment
16.1.2.10. Loss of vulvar subcutaneous fat and hair
16.1.2.11. Diseases related to body system
16.2. Pathologies
16.2.1. Female
16.2.1.1. Perineal herniation
16.2.1.1.1. Result of stretching and tearing of muscles during childbirth, common among older women
16.2.1.1.2. S/S: lower back pain, pelvic heaviness, pulling sensation, urinary and fecal incontinence, retention, constipation
16.2.1.1.3. Nursing interventions: educate on how intercourse can be painful, preparing and informing about surgical repair treatment
16.2.2. Male
16.2.2.1. Benign prostatic hyperplasia
16.2.2.1.1. Most older men have to some degree
16.2.2.1.2. S/S: hesitancy, frequency, nocturia, dribbling, bleeding
16.2.2.1.3. Nursing intervention: prostatic massage, urinary antiseptics, prostatectomy-educate on surgery

