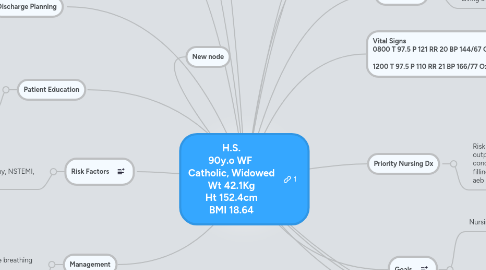
1. Allergies Carbonic Anhydrase Inhibitors Saccharin and Derivatives Sulfa Drugs Thiazide Inhibitors
2. Medications Amlodipine 10mg PO Daily Aspirin 81mg PO Daily Atenolol 25mg PO BID Calcium-Vit D 1 tab PO BID Ducosate 100mg PO BID Hydralazine 2 tab= 50mg PO q8h hydrochlothiazide 12.5mg PO daily
2.1. New node
3. Risk Factors
3.1. Age, Cardiac Hx, Reduced Mobility, PMH: A-Fib, CAD, Mild Dimentia, HTN, Osteoporosis, CABG, Reversed Colostomy, NSTEMI, Chronic LT Hemi-Diaphragm Elevation
4. Discharge Planning
4.1. Pt will need to follow-up with her PCP or cardiologist. She currently lives at an ALF, but requires more assistance than offered there. Social services needs to be contacted to investigate possibly transitioning to a NH and for funding.
5. Management
5.1. IV NS .9% 1000ml, 80ml/Hr Bedrest per RN order Bedpan for bathroom needs HOB elevated 30degrees to facilitate breathing Bed Alarm Medications VS q4 Turn/Rotate q2h
6. Patient Education
6.1. Reinforcement need to educate pt on importance of remaining calm and resting to avoid aggravating her condition. Education on her condition important. Pt has mild dementia and difficulties with short term memory. Her son lives nearby, getting him involved and education for him is important.
7. Medical Diagnosis
7.1. HTN and Syncope
7.1.1. New node
7.2. Pathophysiology
8. New node
9. Outcomes: +2 Peripheral pulses, equal, symmetrical. No bounding or thrills.
10. Diagnostics
11. Lab Values
12. Vital Signs 0800 T 97.5 P 121 RR 20 BP 144/67 Ox 96% RA Pain 0/10 1200 T 97.5 P 110 RR 21 BP 166/77 Ox 96% RA Pain 0/10
13. Key Assessment Findings
13.1. Neuro: Alert, Not oriented to Time, difficulties with short term memory, able to follow simple commands Cardiac: +S1S2, no murmur or thrills, +2 Peripheral Pulses, no JVD, skin WPD, cap refill <2sec Resp: Clear BS LUL RUL, Diminished BS RML LLL RLL, no adventitious BS, no accessory muscle use, DOE GI: Soft, nontender, round, no noticeable abnormalities, Mass RLQ, neg rebound tenderness, hyperactive BS all 4 quadrants, last BM 1/30/12 GU: dysuria, increased frequency w/dribbling, no odor, yellow/clear urine, no burning Integumentary: Warm Dry Intact, no noticeable abnormalities, no edema Musculoskeletal: Limited ROM, unsteady gait with walker assistance, general weakness in extremities (baseline) HEENT: symmetrical, pupils PERRLA, difficulty hearing, glasses for reading, no discharge or other abnormalites noted
13.1.1. New node
14. Psychosocial
14.1. Retired and lives in an assisted living facility, son nearby. Living situation being reevaluated, considering NH. PMH of mild dimentia
15. Goals
15.1. Nursing Intervention 1
15.1.1. Palpate peripheral pulses noting rate, regulartity, amplitude, and symmetry. Document abnormalities and/or deficits.
15.1.1.1. Rationale: Differences in equality, rate, and regularity of pulses are indicative of the effect of altered cardiac output on systemic and peripheral circulation
15.2. Nursing Intervention 2
15.2.1. Provide calm and quiet environment. Review limitations of activities during acute phase.
15.2.1.1. Reduces stimulation and release of stress-related catecholamines, which can aggravate dysrhythmias and vasocaonstriction, increasing myocardial workload.
15.2.1.2. Outcome: Pt will verbalize understanding. Pt will limit activity, remain calm, and not try to get out of bed. Staff will monitor pt frequently to assist with bathroom needs.
16. Priority Nursing Dx
16.1. Risk for fall r/t decreased cardiac output r/t altered electrical conduction, reduced ventricular filling, and increased O2 demand aeb past hx of syncope.
16.1.1. New node
