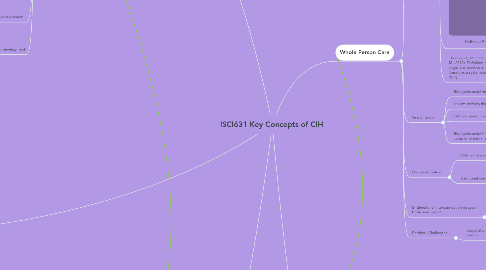
1. Optimal Health
1.1. Definitions
1.1.1. “A state of optimal well-being that is oriented toward maximizing an individual’s potential. This is a life-long process of moving towards enhancing your physical, intellectual, emotional, social, spiritual, and environmental well-being.” (The McKinley Healthy Center at the University of Illinois IL)
1.1.2. “An emphasis on the individuals ability to perform daily activities and more recently to an emphasis on positive themes of happiness...” (Ian McDowell, 2006)
1.1.3. “State of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (World Health Organization)
1.1.4. Eudaimonia; Aristotle
1.1.5. Engagement/ involvement
1.1.6. “…the ability to adapt and self manage in the face of social, physical, and emotional challenges” (Huber et al., 2011)
1.1.7. process / journey not a destination
1.1.8. Tao Te Ching; Lao Tzu
1.2. Search terms
1.2.1. Positive psychology
1.2.2. Psychological well-being
1.2.3. Optimal health environment
1.2.4. Salutogenesis
1.2.5. Allostasis and Allostatic load
1.3. Challenges
1.3.1. Evidence based practitioner concerns
1.3.1.1. Adaptability
1.3.1.2. Nutrition
1.3.1.3. Resilience
1.3.1.3.1. Psychological
1.3.1.3.2. Physiological
1.3.1.4. Optimism vs. Pessimism
1.3.1.4.1. Commitment levels
1.3.1.5. Tongues
1.3.2. Experience based client’s perspective
1.3.2.1. Operational definition
1.3.2.2. Cultural norms
1.3.2.2.1. ‘New’ fitness movements
1.3.2.2.2. Survival vs. luxury
1.3.2.3. Stress management
1.3.2.3.1. Environment
1.3.2.3.2. Personal relationships
1.3.2.3.3. Trauma
1.3.2.4. Personal belief
1.3.2.5. Accessibility
1.3.2.5.1. Historical disenfranchisement
1.3.2.5.2. Policies
1.3.2.5.3. Social welfare
1.4. Relevant research
1.4.1. “On adaptation, life-extension possibilities and the demand for health” (Jon Gjerde, Sverre Grepperud, Snorre Kverndokk; 2001)
1.4.2. “Pathways of emotional autonomy, self-care behaviors, and depressive symptoms on health adaptation in adolescents with type 1 diabetes” (Chia-Ying Chen, Fu-Sung Lo, Bai-Hsiun Chen, Ming-Huei Lu, Yu-Mei Hsin, Rudy-Hsia Wang; 2017)
1.5. Historical development
1.5.1. Hippocratic medicine
2. Evidence Informed Practice
2.1. Definitions
2.1.1. Clinical decisions based on best available evidence integrated with experience of clinician and preferences of patient
2.1.1.1. Begins and ends with the patient
2.1.2. Types of evidence
2.1.2.1. Patient experience
2.1.2.2. Clinical experience
2.1.2.3. Scientific research
2.1.2.4. body of evidence/ iterative process
2.2. Search terms
2.2.1. Evidence-based practice AND patient centered
2.2.2. Evidence informed AND patient centered
2.2.3. Clinical expertise AND patient focus
2.2.4. History of evidence based practice
2.2.5. Evidence informed practice AND patient centered
2.2.6. Whole systems research/ systems pharmacology
2.3. Evidence-based practioner needs:
2.3.1. Comm skills; must understand patient’s background, experiences, preferences
2.3.2. Diagnostic/eval skills
2.3.3. Weigh and synthesize evidence to make decisions in best interest of patient.
2.3.4. Research literacy skills
2.3.5. Clinical skills
2.4. Challenges in finding authoritative references
2.4.1. Limited historical info since this is a 1990’s construct
2.4.2. Limited practical application
2.4.3. based on a drug on model and not on a whole approach
2.4.4. Traditional knowledge is still being explored
3. Patient Practitioner Relationship
3.1. Search terms
3.1.1. "context effect"
3.1.1.1. Influence of context effects on health outcomes: a systematic review Zelda Di Blasi, Elaine Harkness, Edzard Ernst, Amanda Georgiou, Jos Kleijnen
3.1.2. "placebo effect"
3.1.2.1. "Less of a transfer of power …more a symbiotic process where power is created and goes through the relationship (Maizes, Rakel, & Niemiec, 2009, p281)
3.1.3. "healing presence"
3.1.4. "Optimal healing environment"
3.1.4.1. Sakallaris, B. R., MacAllister, L., Voss, M., Smith, K., & Jonas, W. B. (2015). Optimal healing environments. Global Advances in Health and Medicine, 4(3), 40-45.
3.1.5. Definitions
3.1.5.1. Context effect
3.1.5.2. Placebo Effect
3.1.5.2.1. CONTEXT EFFECTS IN WESTERN HERBAL MEDICINE: FUNDAMENTAL TO EFFECTIVENESS? James Snow, MA
3.1.5.3. Healing presence
3.2. Challenges
3.2.1. patients may not have time to invest in long visits
3.2.2. practitioner's belief in the treatment may have a socially transmitted effect on the patient.
3.3. historical context
3.3.1. historically the power difference between patient and practitioner has shifted. Early on the practitioner held the power. Today things are shifting to equalize the relationship.
4. Whole Person Care
4.1. Definitions
4.1.1. Biopsychosocial model
4.1.1.1. George Engel
4.1.1.2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1466742/
4.1.1.2.1. Table 1 Engel’s critique of biomedicine
4.1.2. Holism vs Reductionism
4.1.2.1. The parts of a whole are interconnected and can’t exist or be understood independent of the whole
4.1.3. Thomas, H., Mitchell, G., Rich, J., & Best, M. (2018). Definition of whole person care in general practice in the English language literature: a systematic review. BMJ open, 8(12).
4.1.3.1. "While the terms ‘whole person’, ‘[w]holistic’ and ‘biopsychosocial’ care are sometimes used interchangeably, it is unclear whether they are synonymous, with differences between definitions proposed by general practice organisations."
4.2. Search terms
4.2.1. Biopsychosocial model
4.2.2. Holism systems thinking AND health
4.2.3. “Whole person health”
4.2.4. Biopsychosocial AND complementary medicine
4.2.4.1. An open source paper was just published in 2019. Bevers, K., Watts, L., Kishino, N. D., & Gatchel, R. J. (2016). The biopsychosocial model of the assessment, prevention, and treatment of chronic pain. US Neurol, 12(2), 98-104.
4.3. Historical context
4.3.1. Holism / vitalism
4.3.2. Traditional medicine explanatory models
4.3.2.1. TCM- humans are not seen as body,mind, spirit and soul but as a whole
4.3.2.2. Humans are part of nature
4.4. Bi-directional interconnection between body mind -spirit
4.4.1. Bottom up approach- body affects the mind
4.4.1.1. Tai Chi/Yoga
4.4.2. Top down approach- mind affects the body
4.4.2.1. Mindfulness/meditation
4.5. Barriers / Challenges
4.5.1. scope of practice and dealing with deep trauma
5. Patient Centered Care
5.1. Definitions
5.1.1. Integrative Health
5.1.1.1. “Focuses on patient and importance of patient involvement in their care”
5.1.1.2. Moves focus away from disease and onto the patient as a whole
5.1.2. Patient-centered medicine
5.1.2.1. “Respects the needs and preferences of the individual”
5.1.2.2. “Empowers people to be actively involved in their own healthcare”
5.1.2.2.1. Sharing of power between practitioner and patient
5.1.2.2.2. Patient becomes responsible for their care & health
5.1.2.2.3. four aspects of empowerment
5.1.2.3. Aligns with humanistic medicine
5.1.2.4. Patient values guide all clinical decisions
5.1.3. 5 Principles
5.1.3.1. 1. Respect
5.1.3.1.1. Autonomy/preferences/independence
5.1.3.2. 2. Choice & Empowerment
5.1.3.2.1. Participate to level of ability
5.1.3.3. 3. Pt involvement in Health Policy
5.1.3.4. 4. Access & Support
5.1.3.4.1. Safe and quality care/services
5.1.3.5. 5. Information
5.1.3.5.1. Accurate/relevant
5.2. Search terms
5.2.1. Patient-centered medicine
5.2.2. Person-centered care
5.2.3. Patient empowerment
5.2.4. Patient-reported outcomes
5.2.5. Patient satisfaction
5.2.6. Clinician-patient relationship
5.2.7. Individual Appropriate care
5.3. Challenges
5.3.1. Biomedicine
5.3.1.1. Healthcare workers tend to choose their decision over the patient’s
5.3.1.2. “To be healers, is the point” Don Berwick.
5.3.2. For Practitioner
5.3.2.1. Ensuring access to necessary resources
5.3.2.2. Requires teaching skills/ active listening skills
5.3.2.3. Must collaborate with other practitioners
5.3.2.4. Considering patients preferences and values
5.3.3. Patients
5.3.3.1. Pt has a new responsibility for his/her own health
5.3.3.2. Knowledge/understanding of information provided by practitioners
5.3.3.3. Ability to participate
5.3.3.4. Ability to absorb the information provided
