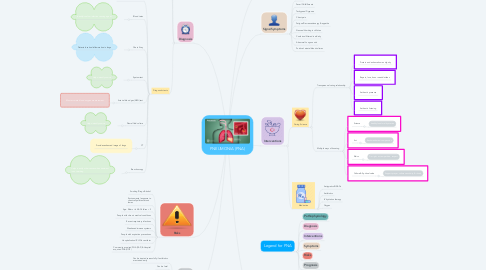
1. Pathophysiology
1.1. Lung Infection caused by bacteria, viruses or fungi
1.1.1. Inflammation of lung air sacks (Alveoli)
1.1.2. Alveoli fill with fluid and pus
1.1.3. Decrease oxygen in blood stream
1.1.4. Causes difficulty breathing
2. Diagnosis
2.1. Medical Exam
2.1.1. Lung sounds
2.1.1.1. Diminished
2.1.1.2. Crackles
2.1.2. Percussion
2.1.2.1. Dullness
2.2. Medical History
2.2.1. Recent travel
2.2.2. Occupation
2.2.3. Exposure to sick people or animals
2.2.4. Any recent illness
2.3. Diagnostic tests
2.3.1. Pulse oximetry oxygen levels
2.3.2. Blood tests
2.3.2.1. Identify/confirm infection causing agent
2.3.3. Chest X-ray
2.3.3.1. Detects location/inflammation in lungs
2.3.4. Sputum test
2.3.4.1. Helps identify source
2.3.5. Arterial blood gas (ABG) test
2.3.5.1. Most accurate blood oxygen measurement
2.3.6. Pleural fluid culture
2.3.6.1. Helps identify source
2.3.7. CT
2.3.7.1. Provides enhanced image of lungs
2.3.8. Bronchoscopy
2.3.8.1. Helps identify other causes when treatment is not working
3. Signs/Symptoms
3.1. Cough
3.2. Fever/Chills/Sweats
3.3. Tachypnea/Dyspnea
3.4. Chest pain
3.5. Fatigue/Decreased energy & appetite
3.6. Nausea/Vomiting in children
3.7. Confusion/Altered in elderly
3.8. Abnormal Lung sounds
3.9. Positive Lactate/blood cultures
4. Risks
4.1. Smoking/Drugs/Alcohol
4.2. Environmental exposure to chemical/pollutants/toxic fumes
4.3. Age: Elders > 64 & Children < 2
4.4. People with chronic medical conditions
4.5. Recent respiratory infections
4.6. Weakened immune systems
4.7. People with aspiration precautions
4.8. Hospitalization/ICU/On ventilator
4.9. Community acquired PNA (CAP) & Hospital acquired PNA (HOP)
5. Prognosis
5.1. Can be treated successfully if antibiotics are started early
5.2. Can be fatal
5.3. Elderly and immunocompromised patients are most vulnerable
5.4. Complications
5.4.1. Respiratory failure
5.4.2. Sepsis
5.4.3. ARDS
5.4.4. Lung abscesses
6. Interventions
6.1. Caring Science
6.1.1. Transpersonal caring relationship
6.1.1.1. Protect and enhance human dignity
6.1.1.2. Repect, love, honor needs/wishes
6.1.1.3. Authentic presence
6.1.1.4. Authentic listening
6.1.2. Multiple ways of knowing
6.1.2.1. Science
6.1.2.1.1. healthy food/oral hydration
6.1.2.2. Art
6.1.2.2.1. Rest/meditation/compassion
6.1.2.3. Ethics
6.1.2.3.1. Do right, act, empathize, respect
6.1.2.4. Culture & Spiritual value
6.1.2.4.1. Support prayer, culture sensitivity, & rituals
6.2. Medication
6.2.1. Antipyretics/NSIADs
6.2.2. Antibiotics
6.2.3. IV hydration therapy
6.2.4. Oxygen
