Ethical Concept Map: Refusal of Recommended Medical Care of a Minor
by Victoria Kirkham
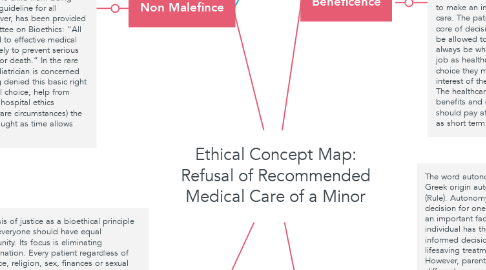
1. Justice
1.1. The basis of justice as a bioethical principle is that everyone should have equal opportunity. Its focus is eliminating discrimination. Every patient regardless of age, race, religion, sex, finances or sexual orientation, to name a few, deserves to be treated equally and with respect. It is so important for not only healthcare providers, but also parents making a choice to approach with an objective point of view and not allow personal feelings to get in the way of providing care. “Perhaps the dedications that is the prerequisite of good parenting stands in the way of making an objectively correct medical decision. For example, parents’ love and dedication for a child needing major surgery may prevent them allowing potentially life-saving surgery because they could not contemplate the pain or disfigurement that their child would suffer. Alternatively, perhaps a parents inability to accept that their child illness would inevitably be fatal would lead them to demand that painful treatment continue long after there was prospect of cure and inflict unpleasant or painful treatment with no advantage to the child”(Baines, 2008). Parenting requires love and dedication, however those commitments may be the blinding in making a rational and just decision.
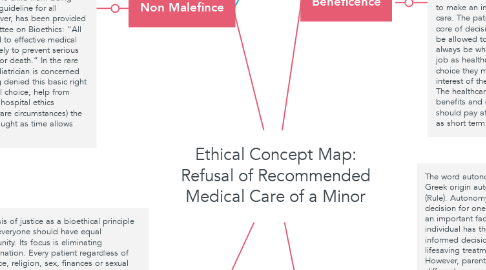
2. Non Malefince
2.1. This means as a medical provider we should do no harm to our patients, and that includes not allowing harm to occur to our patients because of neglect. In this particular situation failure to treat the meningitis will likely result in the child suffering irreversible brain damage or death. By choosing to take the child home in this state with no treatment, the parents are not acting in the child’s best interest, which requires a health care provider to step in to prevent the child from being harmed. “A useful guideline for all pediatricians, however, has been provided by the AAP Committee on Bioethics: “All children are entitled to effective medical treatment that is likely to prevent serious harm, or suffering, or death.” In the rare case in which a pediatrician is concerned that a child is being denied this basic right because of parental choice, help from others, such as the hospital ethics committee and (in rare circumstances) the court, should be sought as time allows (Cummings, 2017).
3. Nursing Code of Ethics: Provision 9. Nurses must make sure to integrate social justice. Social justice covers a wide range of topics. However, as a nurse you have the “ professional responsibility to address unjust systems and structures, modeling the profession’s commitment to social justice and health through content, clinical and field experiences, and critical thought” (ANA, 2015). Nurses should encourage open and honest conversations with their patients as well as their collogues to encourage development. “It is the responsibility of a profession collectively to communicate, affirm, and promote shared value both within the profession and to the public. It is essential that the profession engage in discourse that supports ongoing self-reflection. Critical self-analysis, and evaluation” (ANA, 2015).
4. Victoria Kirkham Erlanger
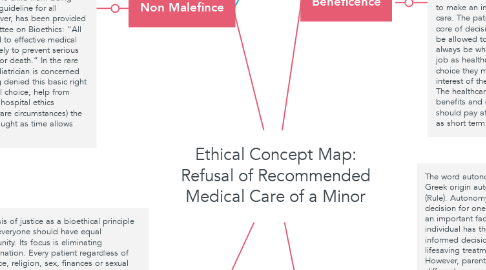
5. Beneficence
5.1. Beneficence as a healthcare provider means acting in the best interest of the patient. As health care providers we should offer to help out patients and educated them to promote a better future. Medicine is an applied form of beneficence, but it is important to remember that so is parenting. “One can see that respect for autonomy and beneficence may at times be in conflict, such as when a competent patient refuses a treatment that would clearly benefit him or her “(Cummings, 2017). Young children are not considered competent, they are unable to make an informed decision regarding their care. The patients best interest should be at the core of decision making process. Parents should be allowed to make a decision, that may not always be what the doctor recommends. It our job as healthcare providers to step in when the choice they make is clearly not in the best interest of the child or could have ramifications. The healthcare team should consider the benefits and drawbacks of any treatment. They should pay attention to long term effects as well as short term.
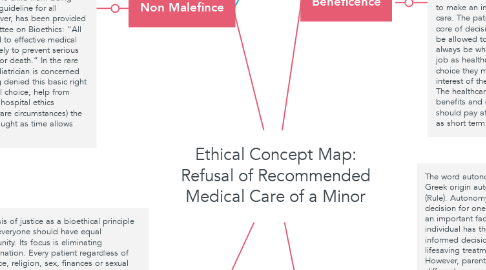
6. Autonomy
6.1. The word autonomy is derived from Greek origin autos (self) and nomos (Rule). Autonomy is the right to make a decision for oneself. In healthcare this is an important factor, because an individual has the right to make an informed decision and refuse potential lifesaving treatment if they wish. However, parental autonomy is different, a competent adult patient can make choices for themselves, but parents refusing necessary medical treatment for their children is not the same. In these situations I feel it is the healthcare providers responsibility to make sure they distinguish between the views and wishes the parents have, and if they are in the child’s best interest. “Their own wishes, however understandable in human terms, are wholly irrelevant to consideration of the objective best interests of the child save to the extent in any given case that they may illuminate the quality and value to the child of the child/parent relationship” (Wilkinson, 2018).
7. Nursing Code of Ethics: Provision 2 A nurses primary commitment is to their patient. This provision reflects the importance of advocating for your patient regardless of age. In this case study the patient in three and unable to make decisions for herself. This means the nurse must advocate for the child and educate the parents in collaboration with the whole healthcare team. “Addressing patients interest requires recognition of the patients place within the family and other relationships. When the patient’s wishes are in conflict with those of others, nurses help to resolve the conflict. Where the conflict persists nurses commitment remains to the identified patient. Nurses may experience conflict arising from competing loyalties in the workplace, including conflicting expectations from patients, families, physicians, colleague, healthcare organizations, and health plans. Nurses must examine the conflicts arising between their own personal and professional values, the values and interests of others who are also responsible for patient care and healthcare decisions and perhaps even the values and interests of the patients themselves” (Ana, 2015). As a nurse it is important to handle conflicts appropriately by focusing on safety and interests of the patient, in doing so a nurse can preserve nursing integrity and whole interprofessional team.