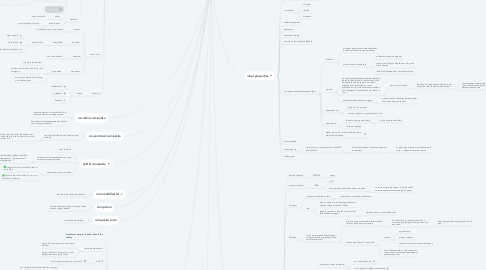
1. composite resin
1.1. low caries risk patients
2. hybrid composite
2.1. most common
2.2. small amount larger particles and small amount microfine particles
2.2.1. improved filler loading (higher % of filler) and coupling agents = improvement in mechanical properties
2.3. advantages over microfilled
2.3.1. elastic limit is almost double that of microfilled
2.3.2. hybrid is almost 3x as hard - so more resistant to abrasion
3. technique
3.1. sufficient polymersiation
3.1.1. hardness of material is half of that of the surface
3.1.2. typically approx 2mm
3.1.2.1. hence 2mm increments in restoration builings
3.1.2.2. bigger than 2mm increments = under polymerised base, early failure
3.1.3. bulk fill
3.1.3.1. claim increments depths up to 6mm
3.1.4. differences between lab and clinical tests
3.1.4.1. can curing light be positioned the same as in a lab
3.1.4.2. can optical rod be placed adjacent to tooth/composite
3.1.4.3. does all blue light illuminate material
3.1.4.4. will composite polymerise (cure) fully
3.1.4.5. what impact does 'stray' blue light have on biological tissue
3.1.5. depth of cure
3.1.5.1. type of composite
3.1.5.1.1. as light hits composite it is reflected, scatters and absorbed. This limits the amount of penetration achieved
3.1.5.2. quality of light source
3.1.5.2.1. designed to produce its maximum light output at approximately 460-480nm (max camphorquinone absorption coefficient is)
3.1.5.3. method used
3.1.5.3.1. tip should be places as close as possible to restoration
3.2. clinical consideration
3.2.1. avoid large restorations
3.2.1.1. larger the restoration = the greater the proportion of polymerisation shrinkage
3.2.1.1.1. so lower chance of creating a good marginal seal
3.2.2. avoid deep gingival preparations
3.2.2.1. can extend sub gingivally (e.g. base of box in root dentine) here it is difficult to ensure close marginal adaptation and to obtain a perfect marginal seal even with DBA
3.2.3. lack of peripheral enamel
3.2.3.1. little enamel left to bond to and so restoration relies more on dentine bond (less effective than acid-etched enamel)
3.2.3.1.1. unrelaible bond
3.2.3.1.2. increases the possibility of breakdown of marginal seal when subjected to stress caused by polymerisation shrinkage, thermal mismatch and occlusal loading
3.2.4. replacement or inlays of load bearing cusps
3.2.4.1. excessive wear of composite likely
3.2.5. poor moisture control
3.2.5.1. impossible to obtain an adhesive bond between the tooth tissues and composite when the tooth surfaces are contaminated by moisture
3.2.6. bruxism
3.2.6.1. Aggressive wearing action associated with bruxism will cause the composite restoration that is in contact with wear down rapidly
4. uses
4.1. used where aesthetics are important
4.2. class III, IV and V permanent restorations
4.3. Class II - when limited occlusal wear
4.4. labial veneers
4.5. inlays, onlays - indirect techniques
4.6. cores
4.7. modified forms as luting cements (some dual cored)
5. classifications
5.1. how
5.1.1. filler type
5.1.1.1. issue if only one size of filler particle
5.1.1.1.1. if only used large filler particle would run out of space and not fill volume, but if put smaller ones then would get more filler particles per unit volume than (better)
5.1.1.2. advantages of adding more filler particles
5.1.1.2.1. improved mechanical properties
5.1.1.2.2. improved aesthetics
5.1.1.2.3. increased abrasion resistance
5.1.1.2.4. lower thermal expansion
5.1.1.2.5. lower polymerisation shrinkage
5.1.1.2.6. less heat of polymerisation
5.1.1.2.7. some radioaque
5.1.2. curing method
5.1.2.1. types
5.1.2.1.1. light cured
5.1.2.1.2. self cured
5.1.2.1.3. UV activation
5.1.2.2. methods
5.1.2.2.1. direct
5.1.2.2.2. indirect/post
5.1.3. area of use
5.1.3.1. anterior
5.1.3.1.1. microfilled or sub micron hybrid
5.1.3.2. posterior
5.1.3.2.1. heavy filled
5.1.3.3. universal
5.1.3.3.1. sub micron hybrid
5.1.3.4. deciduous
5.1.3.4.1. properties
5.1.4. handling
5.1.4.1. classes
5.1.4.1.1. condensable
5.1.4.1.2. syringable
5.1.4.1.3. flowable
6. wear
6.1. material factors affecting wear
6.1.1. filler material
6.1.2. particle size distribution
6.1.3. filler loading
6.1.4. resin formulation
6.1.5. coupling agent
6.2. clinical factors affecting wear
6.2.1. cavity size and design
6.2.2. tooth position
6.2.3. occlusion
6.2.4. placement technqiue
6.2.5. cure efficiency
6.2.6. finishing methods
7. resin modified GI
7.1. used for high caries risk patients
8. compomer
8.1. used for mediaum caries risk, keep under control, regular attnder
9. conventional composite
9.1. strong but problems with finishing and staining
9.1.1. softer the resin the softer the surface and the mote likely to take up stains form food and drinks etc
10. microfine composite
10.1. smaller particles = smoother finsih for better aesthetics for longer period
10.2. but inferior mechanical properties (elastic limit, Young;s modulus)
11. ideal properties
11.1. bonding to tooth/compatible with bonding systems
11.2. mechanical
11.2.1. strength
11.2.2. rigidity
11.2.3. hardness
11.3. thermal properties
11.4. aethestics
11.5. handling/viscosity
11.6. smooth surface finish/polishable
11.7. low polymerisation/setting shrinkage
11.7.1. limitation
11.7.1.1. marginal gap as the composite shrinks away from the cavity wall on setting
11.7.1.2. want as low as possible to
11.7.1.2.1. enhance marginal adaptation
11.7.1.2.2. reduce possibility of breakdown of bond to tooth tissues
11.7.1.2.3. inhibit the development of recurrent caries
11.7.2. process
11.7.2.1. during bonding shrinkage stresses develop because the material is constrained by the adhesion to the cavity walls and these stresses can be sufficient to cause breakdown of the interfacial bond whereby the advantage of an adhesive procedure is lost
11.7.2.1.1. more risk in dentine
11.7.2.2. incremental placement encourgaes
11.7.2.2.1. polymerisation shrinkage towards rather than away from cavity walls
11.7.3. dependent on:
11.7.3.1. type of resin present
11.7.3.2. amount present in unpolymerised form
11.7.4. gap created
11.7.4.1. leads to post op sensitivity
11.7.4.1.1. due to hydroynamic effect
11.7.4.2. marginal leakage
11.7.5. higher proportion of glass filler particles = lower final shrinkage
11.8. biocompatible
11.9. anticariogenic
11.9.1. more prone to secondary caries than GIC and amalham
11.9.1.1. no intrinsic defence mechanisms against caries attack
11.9.1.1.1. so once gap formed, micro-leakage will occur = spread of recurrent caries
11.10. radiopaque
12. components
12.1. glass filler particles
12.1.1. types
12.1.1.1. microfine silica
12.1.1.2. barium aluminium silicate
12.1.1.3. borosilicate glass
12.1.1.4. lithium aluminium silicate
12.1.1.5. quartz
12.1.2. more filller =
12.1.2.1. harder
12.2. resin material
12.2.1. monomers
12.2.1.1. types
12.2.1.1.1. BIS-GMA
12.2.1.1.2. urethane dimethacrylate resin
12.2.1.2. how much reacts
12.2.1.2.1. degree of conversion of resin in only 35-80%
12.2.2. inhibitors used
12.2.2.1. to prevent pre-mature polymerisation (prolong shelf life)
12.2.3. oxygen inhibition surface
12.2.3.1. an air interface with resin
12.2.3.1.1. resin will not cure and sticky surface made
12.3. camphoquinone
12.3.1. initiates free radical addition polymerisation of BIS-GMA
12.4. low weight dimethacrylates
12.4.1. role
12.4.1.1. added to adjust the viscosity and reactivity
12.4.2. example
12.4.2.1. TEGDMA
12.5. silane coupling agents
12.5.1. role
12.5.1.1. allows a bond between filler particle and resin
12.5.1.1.1. if not a good bond between resin and glass then
12.5.2. example
12.5.2.1. y-MPTS
12.5.2.1.1. methacryloxypropyltimemthoxysilane
13. properties specific to composite
13.1. fracture strength
13.1.1. 350MPa
13.1.1.1. strong
13.2. young's modulus
13.2.1. 15GPa
13.2.1.1. rigid
13.2.1.2. amalgam has double the elastic modulus
13.2.1.2.1. so twice as rigid meaning it is twice as able to resist movement when subject to stress
13.3. hardness
13.3.1. referes to materiala surface
13.3.1.1. resistance to scratching, indentation
13.3.2. test
13.3.2.1. identor made of stainless steel that has a specific shape at the end (100g)
13.3.2.2. leave for period of time (30 secs) to allow indentiation to appear
13.3.2.2.1. material is hard = small indentation
13.4. abrasion
13.4.1. when tooth grinds/slides/frictional contact along the opposing tooth surface/restoration
13.4.1.1. results in removal of surface layers when 2 surfaces make frictional contact
13.4.1.1.1. as the surface is removed the resin is removed and the glass filler particles are exposed
13.4.1.2. surface roughness of composite
13.4.1.2.1. causes
13.4.1.2.2. size of filler particles on the surface of composite will determine the degree of surface roughness
13.5. bonding properties
13.5.1. composite bonds to enamel
13.5.1.1. acid etch technqiue
13.5.1.2. so no need for retention undercute
13.5.2. composite bond to dentine
13.5.2.1. through dentine/universal bonding systems
13.5.3. typical bond strength of composite to enamel/dentine
13.5.3.1. 40MPa
13.5.3.1.1. if exceeds 40MPa (e.g. 50MPa+) then likely to debond
13.5.3.2. good bond will reduce micro-leakage and counteract polymerisation shrinkage stress transfer
13.5.3.2.1. polymerisation shrinkage is when the material is trying to pull away from the tooth surface with sufficient force and can break away from the tooth surface - will create gaps
13.5.3.2.2. bonding crucial for stress transfer
13.6. thermal properties
13.6.1. low themal conductivity
13.6.1.1. good
13.6.1.1.1. avoids pulpal damage from hot/cold fluids/foods
13.6.1.2. meaning heat is tranferrred poorly as composite is an insulator not a conductor
13.6.2. high thermal exapnsion coefficient
13.6.2.1. poor
13.6.2.1.1. thermal contraction can occur when cold stimulus and bacteria and saliva can get in
13.6.2.2. enamel = 11; dentine = 8;
13.6.2.2.1. want material to be equal to the tooth
13.7. aesthetic properties
13.7.1. good range of shades
13.7.2. translucency
13.7.3. maintenance of properties over lifetime
13.7.4. resistance to staining
13.7.5. surface finish
13.7.5.1. smooth
13.7.5.1.1. product/technique sensitive
13.7.6. some radiopaque
13.8. handling/viscosity
13.8.1. light cure
13.8.1.1. 'on demand' setting
13.8.2. mixing/working times are dependent on specific materials
13.8.3. different viscosities available
13.9. anticariogenic
13.9.1. generally No
13.10. biocompatibiility
13.10.1. generally though to be OK
13.10.1.1. some concern as not all monomer is polymerised
13.10.1.1.1. overtime the material weakens the monomers could be released resulting in irritation in surrounding tissue
