1. On long use of fluoroquinolones, G -ve bacilli are more resistance.
2. Overview
2.1. Quinolones that are approved for pediatric by FDA in an IV and oral suspension forms.
2.2. 1964 : Nalidixic acid was first approved by FDA for adults, 1980 : approved for children 3 months and olderbut it’s no longer available.
2.3. Fluoroquinolones are active in vitro against both G+ve & G-ve bacteria.
2.4. New chemical modifications resulted in a fluoroquinolones an increased antimicrobial spectrum of activity & better pharmacokinetic properties.
2.5. A policy statement summarizing the assessment of risk & benefits in pediatric patients by AAP in 2006.
2.6. In 2011 : the AAP published an update clinical report because of the increased opthalmic & topical use of fluoroquinolones as well as data on lack of toxicity when use in children.
3. Drugs examples
3.1. Ciprofloxacin , norfloxacin & ofloxacin: have a G-ve spectrum ( pseudomonas ) . In 2004, ciprofloxacin became the first fluoroquinolone approved for use in children from 1 - 17 years.
3.2. Moxifloxacin : displays increased activity against anaerobes while maintaining G+ve & G-ve activity and also has highly activity against mycobacterium tb.
3.3. Levofloxacin : ithas increased activity against many of the respiratory pathogens ex: mycoplasma pneumoniae & chlamydophila pneumoniae; while retaining activity against many of G-ve bacteria.
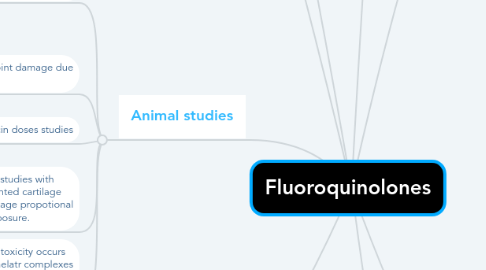
4. Animal studies
4.1. Histopathological
4.1.1. * 90mg/kg/day: SE lasts for two months.
4.1.2. 30mg/kg/day: joint inflammation.
4.1.3. 10mg/kg/day: no SE; but no theraeutic effect.
4.2. Dose dependant: joint damage due to Mg chelation.
4.3. Ciprofloxacin doses studies
4.3.1. 90mg/kg/day, 14 days: arthrotoxicity.
4.3.2. Inflammation lasts fot five months.
4.4. The original toxicity studies with quinolones documented cartilage injury with joint damage propotional to the degree of exposure.
4.5. Data suggest that the toxicity occurs because of forming chelatr complexes with divalent cations mainly Magnesium.
5. Human studies
5.1. All quinolones rarely cause tandon rupture.
5.2. Ciprofloxacin ( 1-17 years): mucoskeletal SE, abnormal liver function, nausea & vomiting, rash, low WBCs count & arthralgia.
5.3. Levofloxacin( pneumonia cases, 6m-19y): joint pain, short hight, and abnormal bone& joint symptoms.
5.4. Fluoroquinolones: peripheral neuropathy & CNS adverse effect ( not commen in children).
5.5. Long-term follow-up study ( cohort study) was published :
5.5.1. * growth impaired or possibly growth impaired, defined as a documented height <80% of the expected height increase 12 months after treatment.
5.5.2. * assessed by the investigators as having abnormal bone or joint symptoms during the original 12 month follow-up.
5.5.3. Persisting musculoskeletal adverse events at the end of the original 12 months of follow-up.
5.5.4. * Follow-up requested by the drug safety monitoring committee because of concerns for possible tendon/joint toxicity associated with a protocol-defined musculoskeletal disorder.
5.6. Although isolate studies of fluoroquinolones drugs have suggested possible musculoskeletal toxicity in children, there is no evidence for long-term harm at this time.
6. Resistance
6.1. MOA:
6.1.1. Mutation leading to change in the target enzymes DNA gyrase & DNA topoisomerase.
6.1.2. Efflux pumps & alterations in membrane porins.
6.1.3. The role of plasmid-mediated quinolone resistance determinants such as qnr genes, continues to increase.
6.2. Resistance is more common among adult cases. ( data from canadian hospitals ).
6.3. Resistance is less common in case of acute use.
6.4. Low dose used for pediatrics are less common with resistance.
7. Considerations/Additional risks
7.1. Fluoroquinolones-class antibiotics are associated with an increased risk of both community-acquired & hospital-acquired C difficile-associated disease.
7.2. Fluoroquinolones may cause cardiotoxicity in adults only.
7.3. May cause Q-T interval prolongation, cardiac disorders, hypokalaemia & hypomagnesemia.
7.4. No cases of cardiotoxicity or torsades de pointes in children associatedwith fluoroquinolones use.
8. Uses of fluoroquinolones in pediatric infection
8.1. Conjunctivitis
8.1.1. An increasing number of topical fluoroquinolones are approved by the FDA for opthalmic ointment for treatment of acute bacterial conjunctivitis in adult and children older than 12 months.
8.1.2. Drugs of choice: levofloxacin, ofloxacin, moxifloxacin, gatifloxacin, ciprofloxacin & besifloxacin.
8.1.3. Conjunctival tissue pharmacokinetic studies that use conjunctival biopsies in healthy adult with besifloxacin, gatifloxacin & moxifloxacin has been performed. All3 agents reached peak concentrations after 15 min.
8.1.4. The utility of agents with higher concentrations is tempered by the observation of a potential increase in ocular adverse events, such as eye pain, and slower corneal reepithelialization.
8.1.5. Better clinical & microbiologic response was noted for besifloxacin compared with placebo,similar outcomes were noted when compared with moxifloxacin.
8.2. External otitis, tympanostomy tube-associated otorrhea
8.2.1. Topical corticosteroids are more effective than acetic acid solutions.
8.2.2. Fluoroquinolones containing preparations represent a safer alternative to treat both otorrhea associated with tympanic membrane perforation & tympanostomy tube otorrhea.
8.2.3. Quinolones and non-quinolones are similar in both microbiologic & clinical cure rates.
8.2.4. Treatment with fluoroquinolones has been well tolerated.
8.2.5. In sever acute otitis externa systemically administered antimicrobial agents should be considered in addition to topical therapy.
8.3. Acute otitis media, sinusitis&lower respiratory tract infection
8.3.1. In AOM, Levofloxacin treatment was well tolerated, with vomiting in 4% of patients documented as the most common adverse effect.
8.3.2. Although fluoroquinolones may represent effective therapy, they aren’t recommended for first line therapy for community_ acquired respiratory tract infection.
8.3.3. In pneumonia, ciprofloxacin therapy has not been uniformly successful in treatment of pneumococcal pneumonia in adults.
8.3.4. Levofloxacin is now recognized as the preferred oral agent for children as younger as 6 months of age with highly penicillin-resistant isolates.
8.4. Uti
8.4.1. The fluoroquinolones remain potential first-line agents only in the setting of pyelonephritis or complicated UTI when typically recommended agents are not appropriate on the basis of susceptibility data, allergy, or SE history.
8.4.2. AAP policy continues to support the use of ciprofloxacin as oral therapy for UTI & pyelonephritis.
8.4.3. If fluoroquinolones starts as empirical therapy but data indicates a pathogen that is susceptible to other class of antibiotics, the therapy can be switched to non-fluoroquinolones agents.
8.5. Mycobacterial infection
8.5.1. The fluoroquinolones are active in vitro against mycobacteria, including M TB & many non-TB mycobacteria.
8.5.2. Increasing multidrug resistance in M TB has led to increased use of fluoroquinolones as part of individualized, multiple drug treatment regimens, with levofloxacin & moxifloxacin showing greater bactericidal activity than ciprofloxacin.
8.5.3. Highlighting that the clinical needs to be aware that additional risk factors for poor wound healing.
8.5.4. Mayincrease the risk of musculoskeletal SE.
8.6. Gastrointestinal infections
8.6.1. Generally, fluoroquinolones are not effective enough in GIT infection.
8.6.2. Salmonella & shigella are resistant to fluoroquinolones agents.
8.6.3. Patients were treated for typhoid fever & invasive non-typhoid salmonellosis clinical & microbiologic success with fluoroquinolones therapy in both adults & children.
8.6.4. In acute invasive diarrhea in febrile children was comparing ciprofloxacin with IM ceftriaxone in a double-dummy treatment protocol, children were treated safety.
8.7. Other uses
8.7.1. Ciprofloxacin & levofloxacin are among the acceptable antibiotics fot use in postexposure prophylaxis againt Bacillus anthracis.
8.7.2. Ciprofloxacin & levofloxacin are used in treatment of many forms of anthrax ( eg: cutaneous, inhalation, systemic ).
8.7.3. Ciprofloxacin is one of the antibiotics options in treatment of plague.
8.7.4. Ciprofloxacin is effective in eradicating nasal carriage of Neisseria meningitidis.
8.7.5. Fluoroquinolones is good penetrating into cerebrospinal fluids ( eg: levofloxacin) by 50%.
8.7.6. Fluoroquinolones is useful in cases of infection after penetrating skin/soft tissue injuries in the setting of water exposure when P aeruginosa or Aeromonas hydrophila.
8.7.7. A recent systematic review of fluoroquinolones therapy for children with fever & neutropenia found good outcomes with short term safety.
