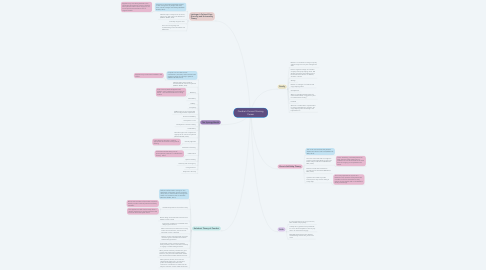
1. Family
1.1. Mother is a coordinator at a large company and has taught me many time management skills.
1.2. Dad is a regional manager of a fertilizer company and enjoys helping others. Did develop necrotizing pancreatitis with no known risk factors as he is not diabetic, alcoholic or obese.
1.3. Siblings
1.4. Brother is a manager of a feed mill and enjoys helping others.
1.5. Grandparents
1.6. When my grandpa passed in 2014 of a massive heart attack, it triggered my love for Cardiovascular nursing.
1.7. Husband
1.8. Works as a medical device representative for a large medical device company. He enjoys helping others and being in the hospital like me.
2. Faith
2.1. It is very important to me to go to church, bible studies and pray daily.
2.2. I always ask my patients if they would like for me to call the chaplain for them or pray with or for them before surgery.
2.3. Read daily devotions that are directed towards being a better wife, person and nurse.
3. Leininger’s Cultural Care Diversity and Universality Theory
3.1. Purpose is to generate knowledge related to the nursing care of people who value their cultural heritage and lifeways (McEwen & Wills, 2019).
3.1.1. Applies to my time being bedside in the Cardiovascular Intensive Care Unit (CVICU), when patient’s either refuse surgery or can not accept blood transfusions due to religious beliefs.
3.2. Identifies major concepts such as culture, culture care, and culture care differences (McEwen & Wills, 2019).
3.3. Culturally congruent care
3.4. Focus is on recognizing and understanding cultural similarities and differences
4. The Synergy Model
4.1. Purpose is to articulate nurses’ contributions, activities, and outcomes with regard to caring for critically ill patients (McEwen & Wills, 2019).
4.1.1. Applies to my current time bedside in the CVICU.
4.2. Identifies eight patient needs or characteristics for critical care patients (McEwen & Wills, 2019).
4.3. Resiliency
4.3.1. Post Coronary Artificial Bypass Graft (CABG), some patients are more willing to follow the recommendations on being mobile.
4.4. Vulnerability
4.5. Stability
4.6. Complexity
4.7. CABG surgery is very complex and the recovery period is very difficult.
4.8. Resource availability
4.9. Participation in care
4.10. Participation in decision making
4.11. Predictability
4.12. Identifies eight nurse competencies appropriate for critical care patients (McEwen & Wills, 2019).
4.13. Clinical judgement
4.13.1. I have become stronger in making appropriate decisions and using critical thinking.
4.14. Facilitation of learning
4.15. Collaboration
4.15.1. I have learned that taking care of post-operative patients is a collaborative nursing effort.
4.16. Systems thinking
4.17. Advocacy and moral agency
4.18. Caring Practices
4.19. Response to diversity
5. Kolcaba’s Theory of Comfort
5.1. Defines comfort within nursing as “the satisfaction of the basic human needs for relief, ease, or transcendence arising from health care situations that are stressful” (McEwen & Wills, 2019).
5.2. Kolcaba’s Propositions of Comfort Theory
5.2.1. Nurses and members of the health care team identify comfort needs of patients and family members.
5.2.2. This applies to a shift I had recently when a patient needed to be comfort measures due to a brain stem and spinal infarct.
5.3. Nurses design and coordinate interventions to address comfort needs.
5.4. Intervening variables are considered when designing interventions.
5.5. When interventions are delivered in a caring manner and are effective, the outcome of enhanced comfort is attained.
5.6. Patients, nurses, and other health care team members agree on desirable and realistic health-seeking behaviors.
5.7. If enhanced comfort is achieved, patients, family members, and/or nurses are more likely to engage in health-seeking behaviors.
5.8. When patients and family members are given comfort care and engage in health-seeking behaviors, they are more satisfied with health care and have better health-related outcomes.
5.9. When patients, families, and nurses are satisfied with health care in an institution, public acknowledgement about that institution’s contributions to health care will help the institution remain viable and flourish.
6. Orem's Self-Help Theory
6.1. The nurse must evaluate the patient’s abilities and level of self-care (McEwen & Wills, 2019).
6.2. The nurse must teach and encourage the patient to take responsibility for their own health and provide self-care (McEwen & Wills, 2019).
6.2.1. This is something I educate patients on daily, because if the patient has no intentions to care for themselves at home then the surgery just completed was a waste.
6.3. Patients must be self-motivated to provide care for themselves (McEwen & Wills, 2019).
6.4. If patients are unable to provide self-care, then they must be willing to accept help.
6.4.1. This is very important in my role as a bedside nurse, because some patients are not able to care for themselves so they require a home health aide or rehabilitation facility at discharge.
