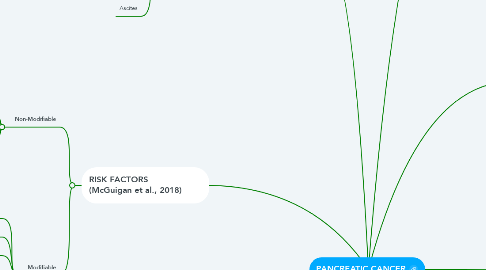
1. RISK FACTORS (McGuigan et al., 2018)
1.1. Non-Modifiable
1.1.1. Age: 90% of newly diagnosed patients are over 55 year of age.
1.1.2. Sex: Worldwide incidence of pancreatic cancer is higher in males than females.
1.1.3. Ethnicity: Within the United States, African Americans have a 50-90% increased risk compared to Caucasians. Higher incidence of modifiable risk factors is one explanation for this disparity.
1.1.4. Family history and genetic susceptibility: Patients with familial risk factors have a 9 times higher risk of developing pancreatic cancer than those with no family history.
1.1.5. Diabetes
1.2. Modifiable
1.2.1. Smoking
1.2.2. Alcohol
1.2.3. Chronic Pancreatitis
1.2.4. Obesity
1.2.5. Diet high in red and processed meats and saturated fats
1.2.6. Infection: Research has shown increased risk in patients with Helicobacter pylori or hepatitis C infections
2. DIAGNOSTIC TESTS (Castillo, 2020)
2.1. Initial testing for patients presenting with jaundice or epigastric pain:
2.1.1. Assay of serum aminotransferases, alkaline phosphatase, bilirubin, and lipase.
2.1.2. Tumor marker CA 19-9.
2.1.3. Abdominal imaging such as CT scan, MRI, and/or PET scan.
2.2. Endoscopic retrograde cholangiopancreatography (ERCP) or a magnetic resonance cholangiopancreatography (MRCP) maybe be given to patients suspected of choledocholithiasis.
2.2.1. Increased risk of complications such as pancreatitis, infections, bowel perforation, and bleeding. Hence, transabdominal ultrasound is the preferred initial test for patients suspected of having pancreatic cancer.
2.3. Biopsy of the pancreas confirms diagnosis of pancreatic cancer.
3. SIGNS AND SYMPTOMS (Castillo, 2020)
3.1. Abdominal pain radiating to back
3.2. Loss of apetitite, fatigue, weight loss
3.3. Jaundice
3.4. Epigastric pain
3.5. Dark urine
3.6. Steatorrhea
3.7. Hepatomogealy
3.8. Ascites
4. TREATMENTS (McGuigan, 2018)
4.1. Surgery: Type of surgery depends on the location of the tumor
4.1.1. Pancreatic Head - Whipple procedure (pancreaticoduodenectomy)
4.1.2. Pancreatic body and tail - Distal pancreatectomy. Spleen may also need to be removed in this case
4.1.3. Total pancreatectomy - requires life-long insulin and enzyme replacement
4.1.4. Vascular resection - often done in conjunction with pancreatectomy for a select group of patients
4.2. Chemotherapy
4.3. Radiation therapy
4.4. Palliative care
4.4.1. Often provided while undergoing surgery, chemotherapy, and/or radiation therapy
5. TYPES (John Hopkins Medicine, 2020)
5.1. Exocrine Pancreatic Cancer
5.1.1. The exocrine gland secretes enzymes that break down carbohydrates, fats, and acids in the duodenum. 95% of all pancreatic cancers are of exocrine origin.
5.1.2. Adenocarcinoma
5.1.2.1. Most common type of pancreatic cancer (90%); occurs in the lining of the ducts.
5.1.3. Squamous Cell Carcinoma
5.1.3.1. Extremely rare
5.1.4. Adenosquamous Carcinoma
5.1.4.1. 1-4% of exocrine pancreatic cancers; agressive with poor prognosis
5.1.5. Colloid Carcinoma
5.1.5.1. 1-3% of exocrine pancreatic cancers; good prognosis.
5.2. Endocrine Pancreatic Cancer
5.2.1. Also known as endocrine or islet cell tumors
5.2.2. Rare; 5% of all pancreatic cancers
6. PATHOPHYSIOLOGY (Hruban, 2020)
6.1. Caused by acquired and inherited mutations in specific cancer-associated genes. These are the main types of mutations:
6.1.1. ACQUIRED MUTATIONS
6.1.1.1. Mutational activation of oncogenes such as KRAS. This mutation occurs in over 90% of pancreatic cancers.
6.1.1.2. Inactivation of tumor suppressor genes such as TP53, p16/cyclin-depedent kinase inhibitor 2A (CDKN2A), and SMAD4.
6.1.1.3. Inactivation of genome maintenance genes such as mutL homolog 1 (MLH1), mutS homolog 2 (MSH2), and mutS homolog 6 (MSH6), which control the repair of DNA damage.
6.1.1.4. Mutated DNA mismatch repair genes, which occurs in 2-3% of pancreatic cancers.
6.1.2. INHERITED/FAMILIAL MUTATIONS
6.1.2.1. Germline (inherited) mutations occur in about 20% of patients with pancreatic cancer.
6.1.2.2. Associated genes include: BRCA2 and BRCA1, PALB2, STK11, ATM.
6.1.2.3. Patients with Lynch Syndrome have inherited mutations in one of several DNA mismatch repair genes and an elevated risk for pancreatic cancer.
6.2. Inflammation
6.2.1. Tumor-elicited inflammation, inflammatory secretions, and infiltrating immune cells play critical roles in cancer initiation, promotion, and progression to malignant metastasis (Shadhu & Xi, 2019). Chronic pancreatitis, or inflammation of the pancreas, is a risk factor for the development of pancreatic cancer.
6.2.1.1. 8 key inflammatory factors are activated in pancreatic cancer, which promote tumor progression:
6.2.1.1.1. NF-B, IL-6, TLRs, TGF-β, TNF-α, IL-1-α, IL-4, IL-8
7. EPIDEMIOLOGY (Dragovich et al., 2020)
7.1. Pancreatic cancer is the the 4th leading cause of cancer deaths.
7.2. It is the 10th most common cancer in men, and the 9th most common cancer in women.
7.3. Approximately 75% of all pancreatic carcinomas occur within the head or neck of the pancreas
7.3.1. 15-10% occur in the tail of the pancreas
8. CAUSATIVE FACTORS (McGuigan et al., 2018)
8.1. DNA gene mutations
8.1.1. Inherited
8.1.2. Sporadic
8.1.2.1. Lifestyle activities that damage DNA, such as smoking or exposure to other carcinogens within the environment
