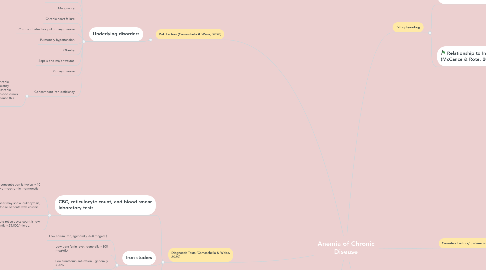
1. Risk Factors (Camaschella & Weiss, 2020)
1.1. Underlying disorders
1.1.1. Infections
1.1.2. Rheumatologic disorders
1.1.3. Inflammatory bowel disease
1.1.4. Castleman disease
1.1.5. Malignancy
1.1.6. Chronic heart failure
1.1.7. Chronic obstructive pulmonary disease
1.1.8. Pulmonary hypertension
1.1.9. Obestiy
1.1.10. Sepsis and major trauma
1.1.11. Kidney disease
1.1.12. Concomitant iron deficiency
1.1.12.1. Some patients with anemia of chronic disease may also have iron deficiency anemia, mainly due to acute or chronic bleeding episodes. Repetitive blood draws for laboratory testing may also cause this (Camaschella & Weiss, 2020).
2. Diagnostic Tests (Camaschella & Weiss, 2020)
2.1. CBC, reticulocyte count, and blood smear laboratory tests
2.1.1. Hemoglobin concentration is typically 10 to 12 g/dL. Normochromic, normocytic anemia.
2.1.2. Peripheral smear may show leukocytosis, especially in those patients with chronic disorders.
2.1.3. Absolute reticulocyte count is low, frequently <25,000/microL.
2.2. Iron studies
2.2.1. Low serum iron, (generally <60 mcg/dL).
2.2.2. Low transferrin level, generally <300 mcg/dL).
2.2.3. Low transferrin saturation, generally <20%.
2.2.4. Ferritin is normal or increased, generally >100 mcg/L.
2.3. CRP and/or ESR
2.3.1. These labs measure measure the general presence of inflammatory disease and are not confirmatory. Both are elevated in cases of anemia of chronic disease.
2.4. Hepcidin level
2.4.1. Level is increased considerably, as it is the primary regulatory of iron availability. Also, hepcidin is inreased in inflammatory conditions.
3. Common Findings/Clinical Symptoms (Weiss et al., 2019)
3.1. Similar to iron-deficiency anemia
3.1.1. Fatigue
3.1.2. Weankess/fainting/feeling dizzy or light-headed
3.1.3. Pallor
3.1.4. Reduced cardiovascular perfomance: tachycardia
3.1.5. Reduced exercise tolerance
3.1.6. Shortness of breath
3.1.7. Impaired learning and memory capacity
4. Pathophysiology
4.1. Anemia of chronic disease results from a combination of (McCance & Rote, 2019):
4.1.1. Decreased erythrocyte life span
4.1.2. Suppressed production of erythropoietin
4.1.2.1. This occurs via the release of inhibitory cytokines IL-1 beta, IFN-gamma, and TNF-alpha.
4.1.3. Ineffective bone marrow erythroid progenitor response to erythropoietin
4.1.4. Altered iron metabolism and iron sequestration in macrophages
4.2. Relationship to Inflammation (McCance & Rote, 2019):
4.2.1. This is a mild to moderate anemia which is present in individuals with conditions of chronic systemic disease or inflammation.
4.2.1.1. As a result, various pro-inflammatory cytokines are released by lymphocytes and macrophages such as TNF-alpha, IFN-gamma, IL-1B, IL-3, and IL-6. These cytokines increase the release of hepcidin.
4.2.1.1.1. Hepcidin is the primary controller of iron availability to developing RBCs. It is a small peptide produced by the liver as a component of the innate immune response to infection (Camaschella & Weiss, 2020). The increase in hepcidin causes iron to be retained within the cells of the reticuloendothelial system. As a result, iron absorption in the small intestine, iron transport across the placenta, and iron release from macrophages are all prevented (Camaschella & Weiss, 2020).
4.2.1.2. Therefore, this type of anemia is also called Anemia of Inflammation.
5. Causative Factors/Epidemiology (Camaschella & Weiss, 2020)
5.1. Second most common cause of anemia world wide, after iron deficiency anemia.
5.2. Multi-factorial causative factors:
5.2.1. Systemic Inflammatory disorders: 30-60% of patients with rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, vasculitis, or systemic sclerosis present with this anemia.
5.2.2. Infections: 18-95% of patients with chronic infections present with this anemia.
5.2.3. Malignancy: More than 30% of cancer patients present with this anemia, especially in hematologic cancers such as lymphoma and multiple myeloma.
5.2.4. Aging: about 1/3 of older adults present with this anemia, often due to inflammatory conditions such as chronic kidney disease.
5.2.5. Chronic disorders: Heart failure, COPD, chronic kidney disease
6. Treatments (Camaschella & Weiss, 2020)
6.1. Initial and preferred treatment:
6.1.1. Treat the underlying inflammatory disorder
6.2. If concomitant iron deficiency anemia is present:
6.2.1. Iron supplementation can be given.
6.3. If severe, life-threatening anemia is present; emergency situation only:
6.3.1. RBC transfusion
6.4. Erythropoiesis-stimulating agents (ESAs):
6.4.1. Only given to patients with chronic kidney disease, select cancer patients receiving chemotherapy, select patients with inflammatory bowel disease or rheumatologic disorders, and select patients who are to have elective surgery.
6.5. New therapies under research:
6.5.1. Hepcidin and ferroportin inhibition/antagonists
6.5.2. Prolyl hydroxylase inhibitors: under investigation for patients who have anemia associated with kidney disease.
