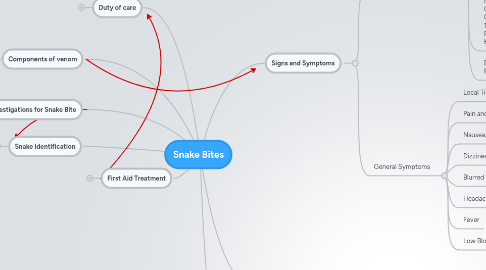
1. First Aid Treatment
1.1. Factors affecting treatment
1.1.1. Snake type and size
1.1.2. Age and general health of victim
1.1.3. Area and tissue that is bitten
1.1.4. Amount of venom injected
1.1.5. Time in which treatment is provided
1.2. First Aid steps
1.2.1. Remove the danger to prevent future attack
1.2.2. Call for help
1.2.3. Keep victim calm
1.2.4. Ensure the bite site is below the heart
1.2.5. Don't let the victim eat or drink
1.2.6. Keep the victim still
1.2.7. First Aid - DRSABC
1.3. Immobilise the limb
1.3.1. Preferably elastic bandage but cloth works
1.3.2. If possible firstly use elasticated bandage over bite site
1.3.3. Wind in overlapping fashion from the distal section of the limb up to pelvic or pectoral girdle
1.3.4. Bandage myst be firm but not so tight that it causes discomfort or to prevents circulation
1.3.5. Splint can be used to further straighten, and immobilise limb
1.3.6. Mark over bandages the area of the bite
1.4. Administer Anti venom Treatment
1.4.1. Only administer when there are significant signs of envenomation of coagulopathy
1.4.2. After initial dose wait 6 hours before administering a second dose
1.4.3. Administer intravenously
1.4.4. Administer according to snake group
2. Snake Identification
2.1. Snake Venom Detection Kit
2.1.1. Bite swab is the most helpful, then urine sample, then whole blood sample
2.1.2. Used to determine which anti venom would be the most appropriate to administer
2.1.3. All medically important snake venoms in Australia can be treated with 5 monovalent anti venoms: Tiger Snake, Black Snake, Brown Snakes, Death Adder, Taipan Snakes
2.1.4. After following the steps, observation of the wells colouring will indicate which anti venom is appropriate
2.1.5. Make sure that the control wells act appropriately or the test is innacurate
2.1.6. If any unexpected results can ring CSL
2.1.7. If no effective result can use polyvalent anti venom
2.2. Note distinstinguishing features of snake and specific symptoms
2.2.1. Red Bellied Black Snake
2.2.1.1. Coagulopathy
2.2.1.2. Myolysis
2.2.2. Tiger Snake
2.2.2.1. Paralysis
2.2.2.2. Muscle Weakness
2.2.2.3. Interferes with blood clotting
2.2.3. Brown Snake
2.2.3.1. Early Cardiac Arrest possible
2.2.3.2. Coagulopathy
2.2.3.3. Renal Damage
2.2.4. King Brown Snake
2.2.4.1. Myolysis
2.2.5. Taipan
2.2.6. Death Adder
2.2.7. Dugite
2.2.8. Copperhead
3. Duty of care
3.1. Once you decide to give first aid, duty of care is established and owed.
3.2. You must continue giving first aid until it is no longer required, medical aid arrives or you are too physically exhausted to continue
3.3. You must provide assistance if you are a driver in an accident, you have a first aid provider role in the workplace or if you have assumed responsibility for another individual and they require first aid
3.4. Ethically, doctors aim to help others lead happy and healthy lives, so while an individual may not be their patient, it would be morally wrong for a doctor not to treat them.
3.5. If you are identified as a doctor you are obligated to provide all the assistance that you can otherwise it is an act of negligence
3.6. Assess your own safety within reason
4. Investigations for Snake Bite
4.1. Blood tests
4.1.1. If no lab test possible, do 'Whole Blood Clotting Test' Test how long it takes to clot against a control
4.1.2. In lab ,test for several things
4.1.2.1. INR - compares clotting time to regular times >2 suggests coagulopathy
4.1.2.2. aPTT
4.1.2.3. Full Blood Exam Platelet count may be decreased in snakebite victim Schitochytes - heamotoxins attacking blood cells White cell count - if raised [leucocytosis] slightly could be snake bite, but high increase suggests other factors (or low lymphocyte levels)
4.1.2.4. Fibrinogen - decreased levels indicate coagulopathy
4.1.2.5. Creatinine and urea indicates renal damage
4.1.2.6. Electrolytes
4.1.2.7. PK for rhabdomyolysis
4.2. Urine tests
4.2.1. Testing for Blood, haemoglobin, myoglobin
4.2.2. Microscopy can confirm whether there are erythrocytes in the urine
4.2.3. Haemolytic toxins in blood can cause damage to blood cells
5. Components of venom
5.1. Prothrombin activating enzymes
5.2. Lipase enzyme
5.3. Postsynaptic Neurotoxins
5.4. Presynaptic neurotoxins
5.5. Hemolysis toxins
5.6. Myotoxins
6. Adrenaline Drug
6.1. Epipen administration 1ml in 1ml ampoule
6.2. Naturally occurring catecholamine
6.3. Increases heart rate, myocardial contraction, irritability in ventricles bronchodilation and peripheral vasoconstriction.
6.4. Used in anaphylaxis, severe asthma, bradycardia, cardiac arrest, cardiogenic shock
6.5. Side effects include anxiety, hypertension, palpitations, tachyarrhythmia and pupillary dilation
6.6. Should be present when giving anti venom
7. Signs and Symptoms
7.1. Snake Specific Symptoms
7.1.1. Taipan Flaccid Paralysis Haemorrhages Incoaguable blood Kidney Failure
7.1.2. Tiger Snake Muscle Paralysis/Weakness Respiratory Failure Haemorrhages Incoaguable blood Kidney Failure
7.1.3. Brown Snake Coagulopathy Collapsing Thrombocytopenia Prolonged Clotting Time Kidney Failure
7.1.4. Death Adder Paralysis is main clinical feature
7.2. General Symptoms
7.2.1. Local Tissue Damage
7.2.2. Pain and Bleeding
7.2.3. Nausea, Abdominal Pain, Vomiting, Diarrhoea
7.2.4. Dizziness, Collapsing
7.2.5. Blurred Vision
7.2.6. Headache
7.2.7. Fever
7.2.8. Low Blood Pressure
8. Serum Sickness
8.1. A reaction by the immune system following exposure to foreign non-human proteins in the blood stream [especially antivenins and antitoxins made in horses]
8.2. Symptoms
8.2.1. Fever
8.2.2. Hives
8.2.3. Itching
8.2.4. Joint pain
8.2.5. Rash
8.2.6. Swollen lymph nodes
8.3. Diagnosis
8.3.1. Blood tests can detect these immune complexities or antibodies and reveal lowered complement levels
8.3.2. Skin biopsy of rash
8.4. Treatment
8.4.1. Costicosteroid creams or ointments to relieve discomfort
8.4.2. Antihistamines can shorten duration of illness, ease rash and itching
8.4.3. Non-steroidal anti-inflammatory drugs may relieve joint pain
8.4.4. Medications causing the sickness must be stopped and future use avoided
