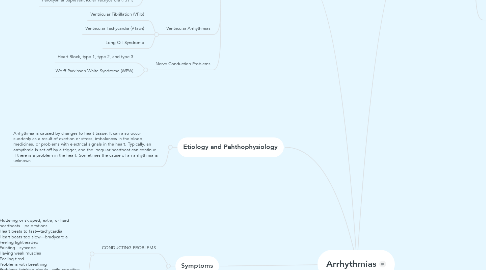
1. Etiology and Pahthophysiology
1.1. Arrhythmia is caused by changes to heart tissue. It can also occur suddenly as a result of exertion or stress, imbalances in the blood, medicines, or problems with electrical signals in the heart. Typically, an arrhythmia is set off by a trigger, and the irregular heartbeat can continue if there is a problem in the heart. Sometimes the cause of an arrhythmia is unknown.
2. Diagnostic Tests
2.1. Heart Monitoring: Holter monitoring, transtelephonic monitoring and implantable loop recording
2.2. Stress test or exercise stress test
2.3. Cardiac catheterization and coronary angiography —To help find blockages in the heart's arteries. Chest x-ray —To see if the heart is enlarged or look for fluid buildup in the lungs. Nuclear scanning—To look at the blood supply to the heart. CT and MRI angiography —To look for blockage of blood flow. Echocardiogram —To check the size, shape, and motion of the heart.
2.4. Blood and urine tests—Used to check your general health. They can also find out electrolytes imbalance or thyroid hormone abnormalities, liver and kidneys function. Tilt table testing —This test is mainly used for people who faint. It can show if there is a problem keeping a healthy blood pressure when changing positions. Electrophysiologic testing —To tests how the rhythm starts and moves through the heart.
2.5. Sleep study —to see whether sleep apnea is the cause of arrhythmia.
2.6. Ultrasound —to diagnose a suspected fetal arrhythmia in the womb.
3. Symptoms
3.1. CONDUCTING PROBLEMS
3.1.1. Fluttering or skipped, extra, or hard heartbeats—palpitations Heart beats to fast—tachycardia Heart beats too slow—bradycardia Feeling lightheaded Fainting—syncope Having weak muscles Feeling tired Problems with breathing Problems thinking clearly—mild cognitive impairment
3.2. ISCHEMIC PROVLEMS:
3.2.1. Chest pain— angina, which may be a symptom of coronary artery disease Feeling tired Problems with breathing Sweating
4. Types of arrhythmia
4.1. Bradyarrhythmia
4.2. Premature Contractions
4.2.1. Premature Supraventricular Contractions/ premature atrial contractions (PAC)
4.2.2. Premature Ventricular Complexes (PVC)
4.3. Sinoatrial Node (SA) Arrhythmias
4.3.1. Sinus Arrhythmia
4.3.2. Sinus Tachycardia
4.3.3. Sick Sinus Syndrome
4.4. Supraventricular Arrhythmias
4.4.1. Atrial Fibrillation (AFib)
4.4.2. Atrial Flutter
4.4.3. Paroxysmal Supraventricular Tachycardia (PSVT)
4.5. Ventricular Arrhythmias
4.5.1. Ventricular Fibrillation (VFib)
4.5.2. Ventricular Tachycardia (VTach)
4.5.3. Long QT Syndrome
4.6. Nerve Conduction Problems
4.6.1. Heart Block, type 1, type 2, and type 3
4.6.2. Wolff-Parkinson-White Syndrome (WPW)
5. Risk Factors
5.1. Age Environment Family history and genetics Race or ethnicity Sex (AF is greater in women) Surgery Lifestyle habits Stress Caffeine Tobacco Alcohol Illegal drugs such as cocaine and amphetamines Diet pills Certain medicines, such as those used to treat a cough or cold Obesity heart problems, asthma, depression, or thyroid problems Other Medical conditions (Aneurysms, Autoimmune disorders, Cardiomyopathy, Diabetes, Eating disorders, Heart attack, Heart inflammation, Heart failure, HTN, Heart tissue abnormalitiesHigh blood pressure, Influenza, or flu, Kidney disease, Heart valves problem, Low blood sugar, lung diseases, Musculoskeletal disorders, thyroid problems, sepsis, and sleep apnea)
6. Treatment and Prevention
6.1. Some arrhythmias you may feel are harmless, but others may cause a stroke, heart attack, sudden cardiac arrest, or death.
6.1.1. lifestyle changes
6.1.1.1. Control fatigue and stress
6.1.1.2. Avoid Triggers, such as nicotine, alcohol, caffeine, OTC meds, and illegal drugs
6.1.1.3. Keep track of pulse
6.1.1.4. Tracking sudden loss of control or faint
6.1.1.5. Regular follow up with cardiac team
6.1.1.6. Managing weight
6.1.1.7. Cardiac healthy eating
6.1.1.8. Being physically active
6.1.1.9. Smoke cessation
6.1.2. medications
6.1.2.1. Class IA Quinidine Procainamide Disopyramide Class IB Phenytoin Tocainide Mexiletine Class IC Flecainide Propafenone Moricizine
6.1.2.1.1. Side effects: Seizures Confusion Mental changes Unwanted heart rhythm changes Nausea Dry mouth Vomiting Diarrhea Constipation Bone marrow damage Clumsiness Vision and hearing changes Rashes Coma
6.1.2.2. Class II: Beta-blockers Propranolol Metoprolol
6.1.2.2.1. Side effects: Breathing problems such as wheezing Feeling tired Heart failure
6.1.2.3. Class III: Bretylium Amiodarone Sotalol Ibutilide Dofetilide
6.1.2.3.1. Side effects: Lightheadedness Nausea Unwanted heart rhythm changes Liver problems (sotalol, amiodarone) Damage to the: Lungs (sotalol, amiodarone) Eyes (amiodarone) Nerves (sotalol) Muscles (sotalol) Thyroid (sotalol, amiodarone)
6.1.2.4. Class IV: Calcium Channel Blockers Diltiazem Verapamil
6.1.2.4.1. Side effects: Lightheadedness Nausea Water retention Damage to liver, kidney, or bone marrow Worsening heart failure Unwanted heart rhythm changes
6.1.2.5. Miscellaneous: Digitalis glycosides Adenosine
6.1.2.5.1. Side effects: Nausea Vomiting Unwanted heart rhythm changes Chest pressure Breathing problems Nausea Flushing Headache Lightheadedness
6.1.3. surgerys
6.1.3.1. Tissue Removal
6.1.3.1.1. Radiofrequency Catheter Ablation: mainly used for atrial flutter , atrial fibrillation (AF) , or ventricular tachycardia (VT).
6.1.3.1.2. Maze Procedures: treat AF
6.1.3.2. Implanted Devices
6.1.3.2.1. Pacemaker
6.1.3.2.2. Cardioverter Defibrillator
6.1.4. Cardioversion
6.1.5. Managing any underlying condition, such as an electrolyte imbalance, high blood pressure, heart disease, sleep apnea, or thyroid disease.

