1. I. Suboptimal Nutrition
1.1. 1. Define suboptimal nutrition, nutritional disorders, malnutrition
1.1.1. Malnutrition
1.1.1.1. Deficiences, excesses, or imbalances in a person's intake of energy and / or nutrients
1.1.1.1.1. Undernutrition
1.1.1.1.2. Overnutrition
1.1.1.1.3. Imbalances
1.1.2. Suboptimal Nutrition / Marginal Deficiency
1.1.2.1. State between adequate and inadequate nutrition intake
1.1.2.2. Less than optimal dose of a nutrient chronically leading to gradual depletion
1.1.2.2.1. Less than DRI
1.1.2.3. No specific deficiency symptoms shown
1.1.2.3.1. Osteoporosis
1.1.2.3.2. Neural Tube Defects
1.1.2.3.3. Fetal Malformations
1.1.2.3.4. Anemia
1.1.2.3.5. BeriBeri (Alcoholics)
1.1.3. Nutrition disorders
1.1.3.1. 1. Dietary intake doesn't contain right amount of nutrients for healthy cellular or physiological functioning
1.1.3.1.1. Changing Nutrient Needs through Lifecycle
1.1.3.2. 2. cannot correctly absorb nutrients from food
1.2. 2. List at least 3 three nutrients of concern for suboptimal nutrition
1.2.1. Nutrients
1.2.1.1. Phytochemicals
1.2.1.1.1. Zoochemicals
1.2.1.2. Shortfall Nutrients
1.2.1.2.1. Vitamin A
1.2.1.2.2. Vitamin E
1.2.1.2.3. Magnesium
1.2.1.2.4. Folate
1.2.1.2.5. Iron
1.2.1.2.6. Potassium
1.2.1.2.7. Vitamin D
1.2.1.2.8. Calcium
1.2.1.3. Food Groups
1.2.1.3.1. Fruits
1.2.1.3.2. Vegetables
1.2.1.3.3. Grains
1.2.1.3.4. Dairy
1.2.1.3.5. Protein
1.3. 3. Identify three causes and/or risk factors for suboptimal nutrition
1.3.1. Causes and Risk Factors
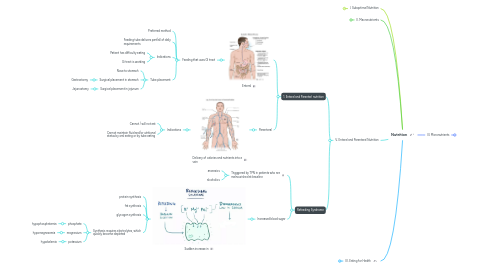
2. II. Macronutrients
2.1. 1. Illustrate 3 Macronutrient disorders, 2. Recognize macronutrient suboptimal nutrition 3. Describe at least 1 nutritional disorder associated with energy and/or macronutrients
2.1.1. Essential Macronutrients
2.1.2. Energy Nutrient/Malnutrition Disorders
2.1.3. Protein Calorie Malnutrition in Industrialized Countries
2.1.3.1. Trauma / illness
2.1.3.2. Marasmus
2.1.3.2.1. COPD
2.1.3.2.2. CHF
2.1.3.2.3. Cancer
2.1.3.2.4. HIV
2.1.3.3. Kwashiorkor-like
2.1.3.3.1. Hypermetabolic acute states/illness
2.1.4. Nutrient Deficiencies / Malnutrition with Bariatric Surgery
2.1.4.1. Protein
2.1.4.2. Iron
2.1.4.3. Vitamin B12
2.1.4.4. Folic Acid
2.1.4.5. Vitamin D
2.1.4.6. Calcium
3. V. Enteral and Parenteral Nutrition
3.1. 1. Enteral and Parenterl nutrition
3.1.1. Enteral
3.1.1.1. Feeding that uses GI tract
3.1.1.1.1. Preferred method
3.1.1.1.2. Feeding tube delivers part/all of daily requirements
3.1.1.1.3. Indications
3.1.1.1.4. Tube placement
3.1.2. Parenteral
3.1.2.1. Delivery of calories and nutrients into a vein
3.1.2.1.1. Indications
3.2. Refeeding Syndrome
3.2.1. Trigggered by TPN in patients who are malnourished at baseline
3.2.1.1. anorexics
3.2.1.2. alcoholics
3.2.2. Increased blood sugar
3.2.2.1. Sudden increase in
3.2.2.1.1. protein synthesis
3.2.2.1.2. fat synthesis
3.2.2.1.3. glycogen synthesis
3.2.2.1.4. Synthesis requires electrolytes, which quickly become depleted
4. IV. Eating for Health
4.1. Popular Diets
4.1.1. Diet Camps
4.1.1.1. High Protein
4.1.1.1.1. Paleo
4.1.1.2. Low Carb
4.1.1.2.1. Keto
4.1.1.2.2. Paleo
4.1.1.3. High fat
4.1.1.3.1. Keto
4.1.1.4. Low Fat
4.1.1.4.1. Pritikin
4.1.1.4.2. Ornish
4.1.1.5. Fasting / Low calorie
4.1.1.5.1. Fasting Diet
4.1.1.5.2. Intermittent Fasting
4.1.1.5.3. Slimfast
4.1.2. Gimmick Diets and Other Diets
4.2. Recommended Diets
4.2.1. 1. Mediterranean Diet
4.2.2. 2. DASH Diet
4.2.3. 2. Flexitarian Diet
4.3. Appropriate tool for identifying good diets
4.3.1. MyPlate
4.3.1.1. 3/4 plate plant sources
4.3.1.2. 1/4 plate animal sources
4.3.1.3. colorful
4.3.1.4. moderation
4.3.1.5. variety
4.3.2. Registered Dietitian
4.4. Types of supplements
4.4.1. Vitamins and Minerals
4.4.1.1. Multivitamins, Vitamin D, Calcium, Vitamin C, Vitamin B/B complex
4.4.2. Specialty Supplements
4.4.2.1. Omega 3 / FAs, Fiber, Probiotics, glucosaomine/chondroitin, CoQ10
4.4.3. Herbals and Botanicals
4.4.3.1. Regular green tea, garlic, cranberry, echinacea, ginseng
4.4.4. Sports Nutrition / Weight management
4.4.4.1. Protein supplement, energy drinks and gels, garcinia cambogia, green coffee, hydration drinks and gells
4.5. Resources
4.5.1. Natural Medicines Database
4.5.2. NIH Supplement Resource
4.6. Drugs that can cause nutrient disorders
4.6.1. PPIs
4.6.1.1. Hypocalcemia
4.6.1.2. Hypomagnesemia
4.6.2. Antacids (Long-Term)
4.6.2.1. Vitamin B 12 deficiency
4.6.3. Antihypertensives
4.6.3.1. Affect body levels of potassium, magnesium, calcium
4.6.4. Cholestyramine
4.6.4.1. Decreased absorption of
4.6.4.1.1. fat-soluble vitamins
4.6.4.1.2. B12
4.6.4.1.3. Folic acid
4.6.4.1.4. Calcium
5. III. Micronutrients
5.1. 1. Illustrate 3 micronutrient disorders 2. Recognize micronutrient disorders 3. Describe at least 1 nutritional disorder/malnutrition associated with micronutrients
5.1.1. Essential Micronutrients
5.1.1.1. Micronutrients from Food Groups
5.1.2. Common Nutrient Deficiencies
5.1.2.1. Iron Anemia
5.1.2.1.1. Causes
5.1.2.1.2. Foods High in iron
5.1.2.2. Vitamin B12 Anemia
5.1.2.2.1. Inability to absorb
5.1.2.2.2. B12 in Diet
5.1.2.3. Folate Anemia
5.1.2.3.1. Inadequate dietary intake
5.1.2.3.2. Folate-rich foods
5.1.2.4. Vitamin D
5.1.2.4.1. Diseases of inadequate Vitamin D
5.1.2.4.2. Poor dietary intake
5.1.2.5. Calcium
5.1.2.5.1. Diseases of Inadequate intake
5.1.2.5.2. High risk groups
5.1.2.5.3. Supplementation to reduce risk of
5.1.2.6. Vitamin D anc Calcium Food sources
5.1.3. Effect of Inflammation on Nutrients
5.1.3.1. :arrow_up: C-Reactive Protein (CRP)
5.1.3.1.1. :arrow_down: Serum B6
5.1.3.1.2. :arrow_down: Vitamin C
5.1.3.1.3. :arrow_down: Vitamin A
5.1.3.1.4. :arrow_down: Vitamin D
5.1.3.1.5. :arrow_down: Folate
5.1.3.1.6. :arrow_up: Ferritin
