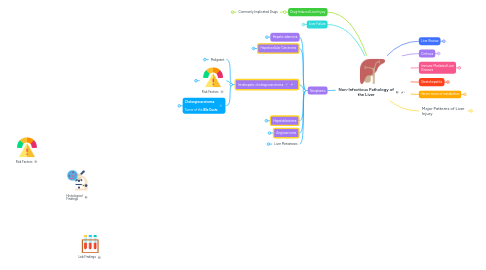
1. Drug-Induced Liver Injury
1.1. Commonly Implicated Drugs
1.1.1. Hepatitis Pattern of Injury
1.1.1.1. Acetaminophen
1.1.1.2. Ketoconazole
1.1.1.3. Valproic acid
1.1.1.4. Isoniazid
1.1.1.5. NSAIDs
1.1.1.6. antidepressants
1.1.2. Cholestasis Pattern of Injury
1.1.2.1. Oral contraceptives
1.1.2.2. Estrongens
1.1.2.3. Tamoxifen
1.1.2.4. Androgens
1.1.2.5. Erythromycin
1.1.2.6. Azathioprine
1.1.3. Cholestatic hepatitis
1.1.3.1. NSAIDs
1.1.3.2. Macrolides
1.1.3.3. Beta-lactam antibiotics
1.1.3.4. Amoxicillin-Clavulanate
2. Liver Failure
2.1. Acute liver failure
2.1.1. 50% DILI
2.1.2. Other causes
2.1.2.1. Acute ischemic injury
2.1.2.2. Acute Budd-Chiari Syndrome
2.1.2.3. Neoplastic infiltration
2.1.2.4. Heatstroke
2.1.3. Clinical Manifestations
2.1.3.1. Encephalopathy
2.1.3.2. Hypotension / Circulatory Dysfunction
2.1.3.2.1. :arrow_down: blood volume
2.1.3.2.2. Adrenal gland insufficiency
2.1.3.3. Renal dysfunction
2.1.3.4. Features by Organ
2.2. Decompensation of chronic liver disease
3. Neoplasms
3.1. Hepatic adenoma
3.1.1. Benign
3.1.1.1. Bland heepatocytes
3.1.1.2. No cytological atypia
3.1.1.3. no blie ducts
3.1.1.4. vessesl without associated connective soft tissue
3.1.1.5. Intact reticulin framework
3.1.1.6. Morphology
3.1.2. Risk Factors
3.1.2.1. Orap contraceptives
3.1.2.2. Anabolic steroids
3.1.2.3. Metabolic disorders
3.1.2.4. Reproductive-age women
3.2. Hepatocellular Carcinoma
3.2.1. Risk Factors
3.2.1.1. 20% Noncirrhotic liver
3.2.1.1.1. Chronic hepatitis
3.2.1.1.2. malginant transofrmation of hepatic adenoma
3.2.1.2. 80% cirrhotic livers
3.2.1.2.1. Chronic HCV
3.2.1.2.2. Steatohepatitis
3.2.2. 40% metastatic disease identified at presentation
3.2.2.1. Lung
3.2.2.2. Bone
3.2.2.3. Abdominal lymph nodes
3.2.3. IHC
3.2.3.1. HepPar1
3.2.3.2. Arginase
3.2.3.3. Glypican
3.2.4. Morphology
3.2.4.1. Mild to marked cytological atypia
3.2.4.2. Benign Liver
3.2.4.2.1. Benign fatty liver, loss of reticulin framework
3.2.4.3. Loss of normal reticulin framework
3.3. Intrahepatic cholangiocarcinoma
3.3.1. Malignant
3.3.1.1. Biliary epithelium
3.3.1.2. Morphology
3.3.1.2.1. Mild to marked cytological atypia
3.3.1.2.2. Prominent growth pattern
3.3.2. Risk Factors
3.3.2.1. Primary sclerosing cholangitis - 5-15%
3.3.2.2. Other
3.3.2.2.1. Hepatolithiasis
3.3.2.2.2. Chronic hepatitis
3.3.2.2.3. Cirrhosis
3.3.2.2.4. Liver Flukes
3.3.2.2.5. Fibropolycystic liver disease
3.3.2.2.6. Ulcerative Colitis
3.3.3. **Cholangiocarcinoma**: Tumor of the **BIle Ducts**
3.3.3.1. Lab Findings
3.3.3.1.1. :arrow_up: LFTs
3.3.3.1.2. Tumor Markers
3.3.3.1.3. :arrow_up: :question: Bilirubin
3.3.3.1.4. :arrow_up: :question: ALP
3.3.3.1.5. :arrow_up: :question: Pancreatic Enzymes
3.3.3.2. Signs / Symptoms
3.3.3.2.1. Obstructive Jaundice
3.3.3.2.2. Pruritis (Extrahepatic)
3.3.3.2.3. Weight loss
3.3.3.2.4. Pain
3.4. Hepatoblastoma
3.4.1. Malignant
3.4.1.1. Epithelial
3.4.2. Most common liver tumor in infants and children
3.4.2.1. 90% of cases Dx before age 5
3.4.2.2. Strong a/w premature birth, low birth weight
3.4.3. Marked elevation in serum AFP - 90%
3.5. Angiosarcoma
3.5.1. Malignant
3.5.1.1. Vascular neoplasm
3.5.1.2. High grade
3.5.2. Third most common primary liver malignancy
3.5.3. Catastrophic intra-abdominal bleeding - 25%
3.5.4. Unkown etiology; a/w occupational vinyl chloride exposure
3.5.5. IHC
3.5.5.1. Vascular IHC Markers
3.5.5.1.1. CD31
3.5.5.1.2. CD34
3.6. Liver Metastases
3.6.1. More common than primary liver tumors
3.6.2. often multifocal
3.6.3. most tumor types can metastasize to liver
3.6.4. Most common
3.6.4.1. Colon
3.6.4.2. Pancreas
3.6.4.3. Lung
3.6.4.4. Neuroendocrine
3.6.4.5. Breast
4. Histological Findings
5. Risk Factors
6. Lab Findings
7. Liver Review
7.1. Liver Functions
7.1.1. Detoxification
7.1.1.1. Drugs
7.1.1.2. Toxins
7.1.2. Bile Salt Synthesis and Secretion
7.1.3. Bilirubin
7.1.3.1. Uptake
7.1.3.2. Conjugation
7.1.3.3. Secretion
7.1.4. Production of Coagulation Factors
7.1.5. Glucose Homeostasis
7.1.6. Iron homeostasis
7.1.7. Production of
7.1.7.1. albumin
7.1.7.2. Globulins
7.1.7.3. Transferrin
7.2. Flow of Blood and Bile
7.2.1. Blood flows in
7.2.1.1. Portal Vein (Primary)
7.2.1.2. Hepatic Artery (secondary)
7.2.2. Blood flows out
7.2.2.1. Hepatic vein into IVC
7.2.3. Bile flows out
7.2.3.1. Hepatic bile ducts
7.3. Hepatic Lobule Microanatomy
7.3.1. Portal Triad
7.3.1.1. Blood flows IN
7.3.1.2. Bile flows OUT
7.3.2. Central Vein
7.3.2.1. Blood flows OUT
7.3.2.2. Bile production begins
7.3.3. Functional Zones
7.3.3.1. Zone 1
7.3.3.1.1. Most resistant to ischemia
7.3.3.2. Zone 2
7.3.3.3. Zone 3
7.3.3.3.1. most sensitive to metabolic toxins
7.3.3.3.2. most susceptible to ischemia
7.3.3.3.3. Site of Bile acid synthesis
7.3.4. Sinusoids
7.3.4.1. Kupffer cells
7.3.4.1.1. Macrophages
7.3.4.1.2. Housed in sinusoids
7.3.4.2. Stellate cells (Ito cells)
7.3.4.2.1. perisinusoidal space
7.3.4.2.2. Fibrinogenesis - Central role
7.3.4.2.3. Store vitamin A
7.3.4.3. Incomplete basememnt membrane, intercellular gaps
7.4. Bilirubin Metabolism
7.4.1. Heme
7.4.1.1. Biliverdin
7.4.1.1.1. (Unconjugated) Bilirubin
7.4.1.1.2. Biliverdin reductase
7.4.1.2. Heme oxygenase
7.4.1.2.1. NADPH + H+
7.4.1.2.2. CO is released
7.4.1.2.3. Iron is released
7.5. Hyperbilirubinemia
7.5.1. Increased Bilirubin production
7.5.1.1. Hemolytic diseases processes
7.5.1.2. Ineffective erythropoiesis
7.5.2. Inefficient conjugation
7.5.2.1. Gilbert Syndrome
7.5.2.1.1. UGT1 mutation
7.5.2.2. Physiologic jaundice of newborn
7.5.2.2.1. Transient low UGT levels
7.5.2.3. Crigler-Najjar syndrome
7.5.2.3.1. Type II
7.5.2.3.2. Type I
7.5.3. Alterations in Excretion of conjugated bilirubin
7.5.3.1. Dubin-Johnson Syndrome
7.5.3.1.1. ABCC2 Mutation
7.5.3.2. Rotor Syndrome
7.5.3.2.1. SLCO1B1/3 Mutation
7.5.4. Obstruction of biliary flow
7.5.4.1. Biliary atresia
7.5.4.2. Mechanical obstruction
7.5.4.2.1. Choledocholithiasis
7.5.4.2.2. Stricture
7.5.4.2.3. Mass
7.5.4.3. Viral hepatitis
7.5.5. Causes of elevated bilirubin levels
8. Cirrhosis
8.1. Entire Liver involved
8.1.1. Fibrous septa subdivide parenchyma into nodules
8.2. Mechanism
8.2.1. Kupffer cells activated following injury
8.2.1.1. Release Cytokines
8.2.1.1.1. Portal fibroblasts activated
8.2.1.1.2. Stellate Cells stimulated
8.2.2. Normal vs Chronic liver
8.3. Progression
8.3.1. Early-Stage
8.3.1.1. Vascular remodeling
8.3.1.1.1. Sclerosis of portal tracts
8.3.1.1.2. Contraction of stellate cells
8.3.1.1.3. Periventricular fibrosis
8.3.2. Late-Stage
8.3.2.1. Vascular changes
8.3.2.1.1. Shunting of blood
8.4. Clinical Manifestations
8.4.1. Liver Damage Effects
8.4.1.1. Hepatic insufficiency
8.4.1.2. Hyperestrinism
8.4.1.2.1. Spider nevi
8.4.1.2.2. Pectoral alopecia
8.4.1.2.3. Gynecomastia
8.4.1.2.4. Altered hair distribution
8.4.2. Portal Hypertension Effects
8.4.2.1. Portal Hypertension per se
8.4.2.2. Hypersplenism
9. Immune-Mediated Liver Diseases
9.1. Autoimmune hepatitis: Type 1: :arrow_up: ANA, ASMA Type 2: :arrow_up: Anti-Liver/-Kidney microsomal-1 *Broad clinical picture from asymptomatic AST/ALT elevations to ALF *
9.1.1. Strong female predominance
9.1.2. Autoantibodies
9.1.2.1. Against hepatocytes
9.1.3. Lab findings
9.1.3.1. ANA :arrow_up: - 80%
9.1.3.2. ASMA :arrow_up: - 70%
9.1.3.3. Polyclonal hypergammaglobulinemia
9.1.3.4. ALP normal or slightly elevated
9.1.3.5. AST and ALT vary
9.1.4. Histologic Features
9.1.4.1. Zone 1 hepatocellular injury
9.1.4.2. Prominent plasma cell population
9.2. **Primary Biliary Cholangitis**: Autoimmune destruction of **Intrahepatic bile ducts** in middle-aged women. *Cholestatic Pattern of Liver Injury * :arrow_up: AMA
9.2.1. Middle-aged female
9.2.2. Lab findings
9.2.2.1. Early Disease
9.2.2.1.1. Bilirubin, AST, ALT - normal or mildly elevated
9.2.2.1.2. :arrow_up: ALP
9.2.2.1.3. :arrow_up: GGT
9.2.2.1.4. :arrow_up: Cholesterol
9.2.2.2. Advanced disease
9.2.2.2.1. :arrow_up: Bilirubin (progressive rise in levels)
9.2.2.2.2. :arrow_up: ALP
9.2.2.2.3. :arrow_up: GGT
9.2.2.2.4. :arrow_up: Cholesterol
9.2.2.3. :arrow_up: AMA - 95%
9.2.2.4. Cholestatic Pattern of Liver Function Test
9.2.3. Histological features
9.2.3.1. Florid duct lesion
9.2.3.2. Dense portal lymphoplasmacytic infiltrate
9.2.3.3. Granulomas
9.2.3.4. Hepatic lobules *undamaged *
9.2.4. Continued injury results in
9.2.4.1. bile duct loss
9.2.4.2. cholestasis
9.2.5. Clinical Manifestations (of progressive cholestasis)
9.2.5.1. Pruritis
9.2.5.2. Jaundice
9.2.5.3. Hyperlipidemia
9.2.5.4. Fat-soluble vitamin deficiency
9.2.5.5. Typical Presentation
9.2.5.5.1. Pruritus + Cholestatic Pattern of Liver Function Test
9.3. secondary biliary Cirrhosis
9.3.1. Uncommon complication of
9.3.1.1. chronic biliary obstruction
9.3.1.1.1. Resultant biliary cirrhosis
9.3.2. Biliary Fibrosis
9.3.2.1. Portoseptal fibrosis
9.3.2.1.1. Caused by the ductular reaction with loss of periportal hepatocytes
9.3.2.2. Eventual linking of portal tracts
9.3.2.2.1. Result of Extension of fibrosis
9.3.2.3. Initial preservation of intrahepatic vascular relationships
9.3.2.3.1. preserved by portal-portal fibrous links
9.3.2.4. Continued loss of hepatocytes leads to
9.3.2.4.1. cirrhosis
9.4. **Primary Sclerosing Cholangitis**: Inflammation / Fibrosis of **Intrahepatic and Extrahepatic Bile Ducts** Most patients have IBD (UC > Crohn) *Cholestatic Pattern of Liver Injury *
9.4.1. Adults 20 - 40, even M:F
9.4.2. Strong association with IBD
9.4.2.1. Ulcerative colitis
9.4.3. Increased risk of
9.4.3.1. cholangiocarcinoma
9.4.4. Hallmark clinical finding
9.4.4.1. Abnormal cholangiogram
9.4.4.1.1. "beaded" appearance of biliary tree on ERCP or MRCP
9.4.5. Lab Findings
9.4.5.1. Liver Biopsy
9.4.5.1.1. Rule out other diseases
9.4.5.1.2. Non-specific or normal findings
9.4.6. Typical Presentation
9.4.6.1. Pruritus + Cholestatic Pattern of Liver Function Test
10. Steatohepatitis
10.1. Defined by 3 components
10.1.1. 1. Steatosis
10.1.1.1. Simple Steatosis on its own is a form of NAFLD
10.1.2. 2. Inflammatory activity
10.1.2.1. Pericellular Fibrosis (Trichrome stain)
10.1.3. 3. Cell injury
10.2. Divided into 2 categories
10.2.1. NASH Inflammatory progression of NAFLD
10.2.1.1. Pathogenesis: Two-hit hypothesis
10.2.1.1.1. 1. Fat accumulation places hepatocytes under stress
10.2.1.1.2. 2. Second insult results in inflammation, cell death, fibrosis
10.2.1.2. Outcomes vary
10.2.1.2.1. Remains stable
10.2.1.2.2. regressing to simple steatosis
10.2.1.2.3. Progressing to cirrhosis
10.2.1.3. Lab Findings
10.2.1.3.1. Liver Enzymes? Poor sensitivity for NAFLD
10.2.1.3.2. ANA
10.2.1.3.3. Imaging studies
10.2.1.4. Histological Findings
10.2.1.4.1. Ballooning hepatocytes
10.2.1.4.2. +/- Mallory-Denk bodies
10.2.1.4.3. Lobular inflammation
10.2.1.4.4. Macrovesicular steatosis
10.2.2. Alcohol-related steatohepatitis
10.2.2.1. Alcohol-induced injury is a multifactorial process
10.2.2.1.1. Primary Mechanism
10.2.2.1.2. Acetaldehyde
10.2.2.2. Risk factors
10.2.2.2.1. Amount of alcohol consumed
10.2.2.2.2. Sex - F > M
10.2.2.2.3. Central obesity
10.2.2.2.4. Patterns of consumption
10.2.2.2.5. Associated medication
10.2.2.2.6. Coffee intake
10.2.2.2.7. Genes regulating expression of proinflammatory cytokines and immune response mechanisms
10.2.2.3. Lab findings
10.2.2.3.1. AST:ALT ≥ 2
10.2.2.3.2. Bilirubin disproportionately high compared to ALP
10.2.2.4. Histological Features
10.2.2.4.1. Identical to NASH
10.2.2.4.2. "Soft" features
10.3. NAFLD (Non-Inflammatory)
10.3.1. Two Primary categories
10.3.1.1. Simple steatosis
10.3.1.2. Steatohepatitis
10.3.1.2.1. NASH
10.3.1.2.2. Alcohol-Related Steatohepatitis
10.3.2. Most common liver disease in western countries
11. Inborn errors of metabolism
11.1. Hereditary Hemochromatosis: Autosomal Recessive Disorder of Increased Iron Absorption :arrow_right: iron overload in tissues.
11.1.1. Autosomal Recessive
11.1.1.1. *HFE* gene mutations
11.1.1.1.1. C282Y gene
11.1.2. :arrow_down: hepcidin synthesis
11.1.2.1. Dysregulated iron homeostasis
11.1.3. Clinical Manifestations
11.1.3.1. 5th or 6th decades
11.1.3.2. Symptoms manifest 2° to
11.1.3.2.1. cirrhosis
11.1.3.2.2. cardiomyopathy / Heart Failure
11.1.3.2.3. Bronze diabetes
11.1.3.2.4. Arthritis
11.1.3.3. Lab Findings
11.1.3.3.1. Transferrin Saturation ≥ 45%
11.1.3.3.2. Ferritin: > 200 (men); > 150 (women)
11.1.4. Pathogenesis of Iron Accumulation
11.1.4.1. Periportal hepatocytes
11.1.4.2. oxidative damage to hepatocytes from excess iron
11.1.4.3. Cirrhosis, fibrosis
11.1.5. Treatment
11.1.5.1. Weekly Phlebotomy
11.1.5.1.1. Monitor serum ferritin levels for efficacy
11.2. Wilson's Disease Autosomal Recessive Disorder of Impaired Copper Transport :arrow_right: Copper overload in **Brain** and **Liver**
11.2.1. Autosomal Recessive
11.2.1.1. *ATP7B* gene
11.2.1.1.1. Transmembrane copper transporting ATPase in hepatocytes
11.2.2. Clinical Manifestations
11.2.2.1. Mean age at Dx: 11-16yo
11.2.2.2. Neuropsychiatric alteration - 40-70%
11.2.2.2.1. behavioral changes
11.2.2.2.2. psychosis
11.2.2.2.3. Parkinsonism
11.2.2.3. Liver disease
11.2.2.3.1. acute, chronic, or rarely acute fulminant hepatitis
11.2.2.3.2. In isolation or in tandem
11.2.3. Lab Findings
11.2.3.1. Liver biopsy
11.2.3.1.1. Copper quantification
11.2.3.2. Screening
11.2.3.2.1. 24-hour urinary copper excretion
11.2.3.3. Serum Ceruloplasmin?
11.2.3.3.1. Acute Phase Reactant
11.2.3.3.2. Can be low in Wilson's but not reliable
11.2.3.4. Slit-Lamp Evaluation
11.2.3.4.1. Kayser-Fleischer rings
11.2.4. Histological Findings
11.2.4.1. Macrovesicular steatosis
11.2.4.2. Vacuolization of nuclei
11.2.4.3. Foci of hepatocyte necrosis
11.2.4.4. Lobular and portal inflammation
11.3. Alpha-1 antitrypsin deficiency: Autosomal Co-Dominant Inheritance Pattern
11.3.1. Clinical Manifestations
11.3.1.1. 4th to 5th decade
11.3.1.2. Liver disease
11.3.1.2.1. 80-90% of PiZZ individuals develop chronic liver disease
11.3.1.3. Childhood Presentation
11.3.1.3.1. cholestatic form of hepatitis in infancy
11.3.2. Autosomal Recessive
11.3.2.1. *SERPINA1* gene
11.3.2.1.1. Transmembrane copper transporting ATPase in hepatocytes
11.3.2.1.2. PiM
11.3.2.1.3. PiZ
11.3.2.1.4. PiZZ
11.3.2.2. Abnormal protein folding AND defects in protein degradation
12. Major Patterns of Liver Injury
12.1. 1. Hepatocellular Injury Pattern
12.1.1. Mild to moderate elevations of AST and ALT
12.1.1.1. < 500
12.1.2. Marked Elevations of AST and ALT
12.1.2.1. > 750
12.1.3. AST/ALT Ratio
