1. Obstructive
1.1. COPD
1.1.1. V/Q decreases (See quick bytes on nptehive.com)
1.1.2. airflow limitation
1.2. Asthma
1.2.1. increased reactivity of trachea and bronchi to stimuli
1.2.2. reversible, dec. FEV1 ( during exacerbation)
1.2.3. narrowing of airways, inflammation, bronchospasm, increased secretion
1.2.4. bronchial sound: high pitch, hollow
1.2.5. V/Q decreases (See quick bytes on nptehive.com)
1.2.6. S/S wheezes, dyspnea, tachycardia, hypoxemia, Inc. Respiratory rate, cyanosis, dec. breath sound, flat diaphragm, Inc. IgE
1.2.7. Drugs: Omalizumab, ipratropium, albuterol, beclamethasone, epinephrine, alupent, ventolin
1.3. Cystic Fibrosis
1.3.1. Genetically inherited
1.3.2. thick secretions of all exocrine glands
1.3.3. Obstructive, restrictive, mixed
1.3.4. Chloride channel block
1.3.5. Decreased ventilation
1.3.6. Test: Blood test-Trypsinogen, positive sweat test, electrolyte test, PFT (Cl>60)
1.3.7. S/s onset early childhood
1.3.7.1. Dyspnea, productive cough, cyanosis, clubbing, crackles, wheeze, anorexia, meconeum ileus, large mucous,
1.3.7.2. 6MWT test is performed for enduarance.
1.4. Bronchiectasis
1.4.1. abnormal dilatation of bronchi
1.4.2. cough & mucopurulent secretions
1.4.3. excess sputum production
1.4.4. frequent secondary infection
1.4.5. Hemoptysis, crackles, cyanosis, clubbing, hypoxemia, dyspnea
1.5. Respiratory distress syndrome
1.5.1. alveolar collapse, dec. pulmonary surfactant
1.5.2. in neonates
1.5.3. s/s respiratory distress, expiratory grunting, flaring nares, crackles, tachypnea, hypoxemia,
1.5.4. Chest X ray: ground glass
1.6. Bronchopulmonary Dysplasia
1.6.1. neonates with RDS, pulm. immaturity & dysfunction due to hyper inflation
1.6.2. Hyperinflation
1.6.3. frequent lower respiratory infection
1.6.4. cor pulmonale, inc. bronchial secretions, crackles, wheezing, low diaphragm
1.7. Emphysema
1.7.1. Permanent abnormal enlargement and destruction of airspaces distal to terminal bronchiles
1.7.2. H/O smoking, chronic cough, sputum
1.7.3. s/s barrel chest, use of accessory muscles, dec. breath sound, dypnea, hyperresonant,
1.7.4. Management: pursed lip, education, endurance exercises.
1.8. Bronchitis
1.8.1. Inflammation of tracheobronchial tree
1.8.2. cough and sputum production lasting atleast 3 months for 2 consecutive years
1.8.3. Wheezing or ronchi
1.8.4. productive mucoid
1.8.5. purulent sputum with infection
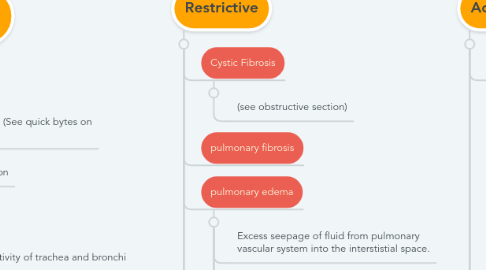
2. Restrictive
2.1. Cystic Fibrosis
2.1.1. (see obstructive section)
2.2. pulmonary fibrosis
2.3. pulmonary edema
2.3.1. Excess seepage of fluid from pulmonary vascular system into the interstistial space.
2.3.2. Cause: left ventricular failure, aortic valvular disease, mitral valvular disease, inhalation of toxic fumes etc.
2.3.3. S/S dyspnea on exertion or paroxysmal nocturnal dyspnea, fatigue, Crackles
2.3.4. PINK FROTHY SPUTUM
2.3.5. Management: Bed rest (head elevation) dec. salt intake
2.3.6. X ray: Hazy opacity, gravity dependent, butterfly pattern.
2.4. ARDS
2.5. abnormal pleura
2.5.1. pleural effusion
2.5.2. pleural fibrosis
2.5.3. pneumothorax
2.5.4. hemothorax
2.6. with neuromuscular disease, connective tissue disorder, neurologic, pregnancy, obesity, ascites
2.7. Atelectasis
2.7.1. Collapsed or airless alveolar unit, hypoventilation
2.7.2. internal obstruction, external compression, low tidal volume
2.7.3. S/S dypnea, tachycardia, increase temp., same side tracheal deviation
2.7.4. increased fremitus
2.7.5. Chest X ray: platelike streaks
3. Acute diseases
3.1. Bacterial pneumonia
3.1.1. Gram positive: acquired via community
3.1.2. gram negative : developed in host(early tissue necrosis)
3.1.3. s/s chills, fever, purulent, blood streaked or rusty sputum, inc. WBC, Dec., bronchial breath sounds, crackles, hypoxemia, hypocapnea initial
3.2. Viral pneumonia
3.2.1. Inflammation caused by viral agents, influenza, adenovirus, cytomegalovirus, herpes, measels
3.2.2. S/S fever, chills, dry cough, dec. breath sounds, crackles, hypoxemia, hypercapnea, wbc normal, headache
3.3. Tuberculosis
3.3.1. Mycobacterium tuberculosis
3.3.2. infection spread by aerolized droplets
3.3.3. incubation 2-10 weeks
3.3.4. primary disease lasts 10 days to 2 weeks
3.3.5. S/S Fever, weight loss, cough, hemoptysis, night sweat, blanching, dyspnea, chest pain, increased lymphocytes
3.3.6. Precautions: Airborne (isolation)
3.3.7. medication: 3-12 months
3.3.8. drugs: Isoniazide, rifampin, ethambutol, pyrazinamide
3.3.9. Skin test: Mantoux test
3.4. Aspiration Pneumonia
3.4.1. Usually in patient with dysphagia (Parkinson, Multiple sclerosis), fixed neck extension, intoxication, impaired consciousness, recent anesthesia, neuromuscular disease.
3.4.2. S/s symptoms after aspiration event, cough dry at onset, progress to putrid secretion, dyspnea, tachypnea, cyanosis, wheezes, crackles, fever.
3.5. pnemocystis pneumonia
3.5.1. fungus (pneumocystis carinii)
3.5.2. in immunocompromised host
3.5.3. S/S Shortness of breath, non productive cough, crackles, weakness, fever, confusion

